TROUBLESHOOTING IN INFERTILITY PROBLEMS IN CATTLE & ITS SOLUTION
Compiled & shared by-DR. RK SINGH, JAMSHEDPUR
Animal’s reproductive ability is one of the key elements in a dairy herd. Production of one calf crop per year provides maximum profit to the dairy farmers. Good reproduction and good production are just like two sides of a coin for making the dairy enterprise profitable.
The productive life of a cows starts with parturition which is the chief event of reproduction. After that the cow needs regular cycles of conception and calving to begin consequent lactation which is the key component of her productive life. Hence, for a successful dairy farming reproductive performance of the dairy animals play a very crucial role. Therefore, the reproductive problems that ultimately leads to reproduction failure needs to be diagnosed and checked as early as possible for optimal production and profit in the farm.
One of the major loss making reproductive problems in dairy cattle prevalent at field level is existence of a large number of repeat breeder cows. A repeat breeder is a cow that has normal estrous cycle, is free from palpable clinical abnormalities, has no abnormal vaginal discharge, is less than 10 years old, has calved at least once but has failed to conceive after at least three or more consecutive inseminations. In a simpler term, in case of repeat breeding cows will come to heat regularly but not succeed to conceive after successful mating. Repeat breeding causes financial loss in terms of repeated inseminations, treatment, cost of feeding without production, production loss due to delayed conception.
Repeat Breeding:
High Incidence of Cows Requiring Three or More Services
Possible Causes
- Improper timing of insemination—breeding too early or too late.
- Frequently inseminating cattle based on secondary signs of estrus.
- High incidence of uterine infection.
- Improper insemination technique or use of semen damaged during storage or handling.
- Embryonic or fetal mortality.
- Excessive weight loss or poor body condition.
- Improper palpation technique during pregnancy exams.
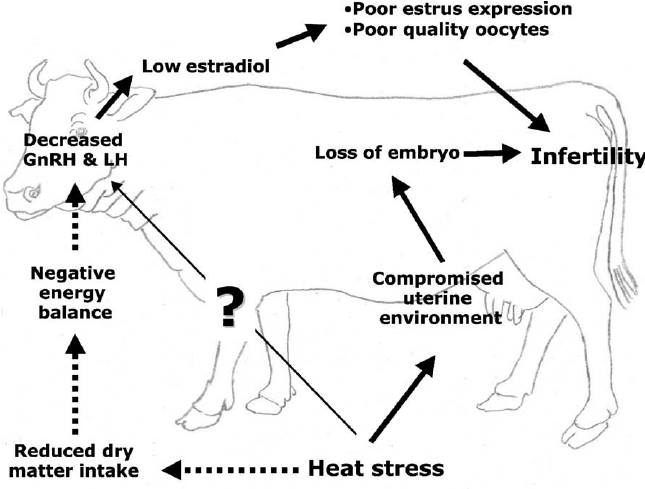
- Heat stress.
- Inseminating cows too late in relation to ovulation.
- Deficient crude protein or excess degradable protein intake.
- Gross over-conditioning.
- Diseases
- Subclinical uterine infection.
- Vibriosis and trichomoniasis in natural breeding.
- Leptospirosis and haemophilus.
- Viruses (IBR/IPV, BVD) and maybe others.
- Ureaplasma and mycoplasma.
- Toxicity (i.e., ketone bodies, mycotoxins, high blood urea nitrogen (BUN) and endotoxins).
- Imbalance of calcium, phosphorus, vitamins A, D, and E and carotene.
- Hormonal imbalance (i.e., intake of forages high in estrogen).
- Use of low breeding efficiency sires.
- Improper use of drugs or hormones that impact reproductive function.
Suggestions
- Evaluate the heat detection program and timing of service.
- Use Milk Progesterone Testing to evaluate accuracy of heat detection.
- Submit blood samples or reproductive tract swabs for disease testing.
- Have veterinarian examine repeat breeders; treat if infection is present. (See suggestions for uterine infection, page 3).
- Re-evaluate semen handling and insemination techniques. Attend retraining session for artificial insemination technique.
- Analyze milk samples for milk urea nitrogen (MUN) through local DHIA service center. Submit blood samples for CBC (complete blood count), including serum minerals.
- Test forages and the total mixed ration (TMR) for standard analysis, minerals and mycotoxins if suspected.
- Submit feeding program for evaluation and check basic feeding practices (i.e., feed availability).
- Avoid gross overfeeding of grain.
- If possible, provide cows with adequate amounts of fresh forage as pasture or greenchop for at least four to six weeks each year.
- Avoid moldy or apparently high-estrogen forages.
- Purchase semen from reputable sources.
- Review use of drugs and/or hormones administered to breeding stock.
- Evaluate vaccination and biosecurity practices and protocols.
Anestrus
Estrus is not Exhibited or Estrus is not Observed
Possible Causes
- Undetected heat symptoms in normal cow.
- Failure to properly observe for estrus.
- Failure to keep adequate records.
- Failure to turn cows out of stanchion barns.
- Few open cows within a group that are available to detect heat in other open cows—pregnant cows and cows in midcycle are much less likely to mount cows in or near heat.
- Feet and leg problems, lameness.
- Slippery footing.
- Unfamiliarity with symptoms of estrous behavior.
- Quiet heats or silent heats (normal ovulation with little or no sign of heat).
- True anestrus: estrus is not occurring.
- Energy deficiency, cows losing large amounts of flesh due to high milk production and/or underfeeding and low dry matter intake.
- Anemia, often from inadequate protein, iron, selenium or vitamin E.
- Phosphorus deficiency, especially in heifers or excess phosphorus.
- Poor endocrine tone from stored forage only, no fresh forage; lack of fat-soluble vitamins, plant hormones and antihormones.
- Pyometra and severe uterine infection. Cows may or may not show discharge and generally do not cycle.
- Cystic ovarian disease—70% of cystic cows are anestrus.
Suggestions
- Examine suspect cows to determine whether they are truly anestrus, i.e., absence of ovarian structures, cysts, pyometritis, etc.
- Maintain adequate reproductive records and use heat expectancy chart. Milk Progesterone Testing can be used to evaluate heat detection.
- Closely observe cows for heat for at least 20 minutes each time. More heats will be shown in evening and early morning than at mid-day. Provide good footing in heat detection area.
- In conventional housing situations, turn cows out at least daily. Determine which cows are pregnant and concentrate efforts on open cows.
- Use heat detection aids.
- Check problem cows for anemia:
- Run CBC, which includes hemoglobin, packed cell volume, red and white blood cell counts.
- Submit unclotted samples from 12 to 21 cows, including dry cows and early lactation cows. Use a local hospital, veterinary clinic or a PA Animal Diagnostic Lab for blood determinations.
- Check serum mineral, protein and BUN or MUN levels. Submit 2 tubes of clotted blood per cow or 10 cc of serum per cow. Sample about 12 to 21 cows. Do not sample treated cows, those within one week of expected calving or those fresh less than three weeks. Forward samples to an animal diagnostic laboratory.
- Submit forage and/or TMR samples for standard analysis and mineral tests.
- Submit feed program for evaluation. Carefully examine protein, mineral and vitamin levels.
- Examine cows for uterine infection. Prevent retained placenta and reproductive tract infections as given on pages 3 and 4.
- Whenever possible, have cows in a gaining condition as desired breeding time approaches.
- Control periparturient disease problems, especially ketosis.
- Provide cows with adequate amounts of fresh forage for at least four to six weeks each year.
- Ensure pregnancy exams are conducted routinely, 40 to 50 days after breeding.
- Treat for anemia if determined to be a problem.
Cystic Ovaries
Possible Causes
- Too many problems during calving or early lactation such as dystocia, milk fever, retained placenta, severe mastitis and uterine infection.
- There is evidence to suggest a heritable component to cystic ovaries.
- High milk production is an unlikely cause.
- Inadequate intake of vitamins A and E, carotene or selenium.
- Wide Ca:P ratio or over-supplementation with calcium is a remote cause.
- High dietary estrogens from moldy feeds or legumes (fresh forages, such as alfalfa, birdsfoot, ladino and white clover) that have high levels of estrogen compared to other forages.
Suggestions
- Control periparturient disease problems and metabolic disorders. Avoid exposing cattle to a stressful environment.
- Evaluate affected cows to determine if there is a heritable trend; cull cows accordingly.
- Examine feeds for mold. If present, test for mycotoxins.
- Submit forage samples for standard and mineral tests.
- Submit feeding program for evaluation.
- Avoid feeds likely to be high in estrogen-like compounds.
Reproductive Tract Infections
Possible Causes
- Improper dry cow nutrition.
- Contamination at calving due to unsanitary calving area; virulent organisms in calving area and unsanitary human interventions at calving time.
- Dystocia and retained placenta (see page 4).
- Actinomyces pyogenes, Mycoplasma bovigenitalium, Haemophilus somnus, ureaplasma, and the bovine herpes viruses, infectious bovine rhinotracheitis (IBR) and infectious pustular vulvovaginitis (IPV) cause vaginal and uterine infection.
- Unsanitary examinations or insemination technique.
- Over-conditioning at calving relates to a higher incidence of infections. Low levels of calcium may contribute to retained placenta, which may develop into uterine infection.
- Selenium and vitamins A or E deficiencies.
- Inseminating cows not in true heat.
- Damage to tract from difficult calving or damage during insemination.
- Venereal infection, especially trichomoniasis, spread by natural service, which causes severe uterine infection.
- Poor quality water from a contaminated well or other water source.
- Routine use of uterine boluses or infusion may cause sterile pus condition or increase infections.
Suggestions
- Evaluate dry cow nutrition.
- Calve cows in a clean and sanitary environment:
- Use reasonably clean outside paddocks or fields during good weather.
- Clean, sanitize and re-bed maternity pens or calving areas after each calving.
- If uterine infection is a chronic problem, rest calving areas for one to two months. Calve cows in a new, clean site.
- Reserve maternity pens for calving only.
- Reduce incidence of retained placenta if it is a problem. See page 4 for details.
- Have your veterinarian culture and/or blood test infected cows and recommend treatment.
- Keep insemination equipment clean and make a clean entry into the reproductive tract.
- Using a protected sheath or double-rod technique of insemination has been effective in chronically infected herds.
- Administer injectable selenium-vitamin E preparation at least 21 days prior to expected calving.
- Have cows examined carefully three to four weeks after freshening and treat if necessary.
- Don’t use natural service when there is any indication of reproductive tract infection. The bull may further spread the disease without showing symptoms.
- Don’t inseminate cows showing abnormal discharges.
- Test water quality.
Abortions
Possible causes of early abortions (six to seven months or sooner)
- Vibriosis or trichomoniasis—more apt to occur with natural breeding.
- Leptospirosis, haemophilus and other diseases causing high fever.
- Viral diseases, IBR and BVD.
- Silo gas, severe nitrate or prussic acid poisoning and toxic plants.
- Mycotic infections.
- Selenium and vitamin E deficiency.
Possible causes of late term abortions
- Brucellosis and salmonella.
- Vitamins A and E, selenium and iodine deficiency.
- Viral diseases, IBR and BVD.
- Silo gas, nitrate or prussic acid poisoning, toxic plants and mycotic infection.
- Use of cortisone or prostaglandin in pregnant cows.
- Domestic pets spreading infectious agent among cattle.
Suggestions (try to determine and eliminate causes)
- Conduct blood testing for brucellosis, leptospirosis, IBR, BVD, haemophilus and neospora.
- Take necropsy of fresh fetus and placenta to a diagnostic lab.
- Closely observe environment, including pastures with nitrate accumulating weeds and water sources.
- Submit vaginal swabs on culturettes with Amies media for ureaplasma, mycoplasma and possibly vibrosis and trichomoniasis infection.
- Evaluate feedstuffs for nitrates and mycotoxins.
- Evaluate ration for selenium, iodine and vitamins A and E.
- Quarantine new additions to the herd.
Retained Placenta
Possible Causes
- Abnormal parturition (i.e., dystocia, premature birth, excessively large fetus, Cesarean section or uterine tension, stillbirth, abortion, early births and toxins).
- Uterine inertia; hypocalcemia (milk fever) and dystocia.
- Selenium deficiency.
- Vitamins A and E or carotene deficiency; high-hay ration, poor quality forage or lack of fresh forage.
- Specific infections (brucellosis, IBR, BVD, leptospirosis and neospora); calf usually aborted or stillborn; contagious.
- Non-specific infections (salmonella, fungus, and Actinomyces pyogenes); placental infection; calf usually aborted or stillborn; not contagious.
- Over-conditioned cows; excessive corn silage fed to dry cows (over 50% of forage dry matter intake).
- Overfeeding grain to dry cows (greater than 0.5% of bodyweight).
- Excessive calcium from too much legume forage fed to dry cows (over 25-30% of forage dry matter intake).
- Calcium and phosphorus deficiency; inadequate supplementation for dry cows.
- Excessive vitamin D (over 50,000 to 100,000 units daily).
Suggestions
- Minimize stressful conditions during dry period and at calving.
- Prevent milk fever.
- Evaluate dry cow ration.
- Provide 0.3 part per million selenium in total.
ration dry matter for both milking and dry cows. If the problem affects the entire herd, submit blood samples from six to 12 dry cows for calcium, phosphorus, magnesium, selenium (glutathione peroxidase), vitamins A and E, carotene and BUN analysis.
- If special supplementation is not used for dry cows, administer 50 mg of selenium and 680 units of vitamin E as an injection about three weeks before calving.
- Ensure adequate vitamins A and E equivalent intake:
- Provide about 135,000 total units of vitamin A for dry cows and 150,000 for milk cows; 2,000 to 3,000 units of vitamin E for dry cows and 1,000 to 1,500 units for milk cows total daily from all sources (natural and supplemental) with 1 mg of carotene equivalent to 400 units of vitamin A.
- Provide cows with fresh forage as green- chop or pasture for at least four to six weeks each year.
- If there are numerous abortions, test the herd for brucellosis, neosporosis, IBR, BVD, leptospirosis and non-specific infections.
- Prevent cows from becoming over-conditioned.
Difficult Calvings
Possible Causes
- Large calves can result from overfeeding late in pregnancy.
- Underfeeding heifers before calving and/or during first two lactations, heavy parasite load, lack of skeletal development and small pelvic area.
- Milk fever, ketosis and other complications at parturition.
- Fetal abnormalities.
- Neglect of freshening cow.
- Over-conditioning of older cows or heifers leads to excessive fat deposits in the birth canal.
Suggestions
- Breed heifers to calving ease sires.
- Carefully monitor growth of heifers before and after breeding.
- Feed milking heifers for growth as well as maintenance and production.
- Control parasites in young stock.
- Control milk fever and other freshening problems (refer to extension publication on Trouble Shooting Milk Fever and Downer Cow Problems).
- Avoid getting cows too fat, especially during late lactation and the dry period.
- Attempt to alter time of calving by feeding dry cows during the late afternoon or early evening hours so more calvings occur between morning and early evening.
Heifer Breeding Problems
- Delayed sexual maturity from underfeeding energy or protein and parasitism.
- Weak or silent heats from:
- Lack of heat detection.
- Underfeeding energy.
- Anemia from parasites or faulty nutrition (low protein, selenium, vitamin E or iron).
- Phosphorus deficiency.
- Lack of vitamin A from deficient intake of vitamin A, carotene or phosphorus.
- Genital abnormalities:
- Freemartin—failure of reproductive tract to develop.
- Closed cervix or blocked oviduct.
- Infantile reproductive tracts.