Blood in Milk (Hemolactia) in Cows and Buffaloes : Causes, Diagnosis and Treatment
Blood in the milk is called as haemolactia or haemogalactia. In normal physiological state, hemolactia is occurred at the end of lactation or first few days of lactation and this will not be continued more than 14 days. Hemolactia is due to various aetiologies. Hemolactia is due to diapedeis in the alveoli of mammary gland. This occurs frequently immediately after calving and this may occur at any lactation stage. Therefore, higher quantity of RBCs is available in the milk as look as reddish or pinkish milk and red cream and red sediment at the bottom. On the other side, harsh milking by hand or machine causes damage of the epithelial lining in the teat cistern inturn induce haemorrhage by diapedeis is considered as pathological (Heidrich and Renk, 1967). Trauma or injury in udder and teat is another common cause of hemolactia.Dark brown coloured or as like uncloated venous blood in the udder section indicates severe haemorrhage from a major vein of the udder, which is another cause of hemolactia (Ayaz, 1999). Pendulous and severe udder edema especially in high milk producing cows predispose to hemolactia.
Dairy farmers frequently approach practicing veterinarians for the treatment of cows or buffaloes producing milk which is reddish or pinkish due to the presence of blood. Farmers suffer from the economic loss because bloody milk is often rejected by the consumers. The condition is usually sporadic in occurrence but rarely several lactating animals may be affected at a time.
Causes
There are several causes of blood in milk. The important causes of this disorder are briefly described below:
- Hemorrhage: Hemorrhage by diapedesis (i.e. passage of blood cells through capillary walls into the tissues), in which RBCs are present in the alveoli of mammary gland, occurs quite frequently just after calving. Hemorrhage due to diapedesis may also occur at any stage during the lactation. Sometimes, the number of RBCs in the milk may be so numerous as to give the milk a pinkish tinge and cause red cream and Typically, however, the number of RBCs in the milk is quite low and the milk may have only a slight reddish or pinkish tinge. Due to congestion (hyperemia) of the udder and teat at calving, the udder tissue is uniformly reddened, and extravasation of blood into the interstitium may be demonstrated microscopically. A slight admixture of blood after calving is considered to be physiological and does not persist longer than 14 days at the most. Any other hemorrhage by diapedesis is considered to be pathological and results from damage to the epithelial lining of the teat cistern, owing to harsh milking by hand or machine (Heidrich and Renk, 1967). Trauma to udder and teat is one of the common causes of blood in milk due to hemorrhage. The udder secretion may be dark brown like venous blood without tendency to clot when hemorrhage from a major vein of the udder is the cause of bloody milk (Ayaz, 1999). Severe udder edema and a pendulous condition of udder may predispose to appearance of blood in milk.
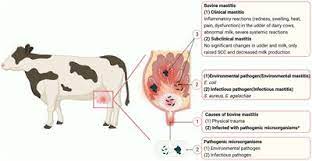
- Systemic microbial infections: Several infections including those caused by some bacteria (leptospira spp, Brevibacterium erythrogenes, Serratia marcescens, Micrococcus cerasinus, Micrococcus chromidrogenes rubber, Micrococcus roseus, Lactorubefaciens gruber, Sarcina rubra ), some viruses and red yeast(Monascus purpureus) may cause systemic infections associated with intravascular hemolysis and capillary damage in udder leading to reddish or pinkish discoloration of milk (Balhara et al., www.buffalopedia.cirb.res.in/)
Leptospirosis is one of the common causes of blood in milk in dairy animals. When leptospirosis is the cause of bloody milk, the milk from all 4 teat would be red in colour, thick in consistency and it contains blood clots and milk clots. Flaccidity (= softness) of udder is another characteristic clinical feature of leptospiral mastitis (‘cold mastitis’ i.e. mastitis with no sign of inflammation). Nonspecific signs include fever, hemoglobinuria, abortion, decrease in appetite and milk yield. After showing these signs for a few days, the animal would develop mastitis (Champawat et al., 1984.)
Feeds containing natural toxins or dyes: Sometimes, reddish discoloration of milk is due to feeding of fodders belonging to family Rubiaceae (dyer’s madder, Rubia tinctorum). Certain plant toxins present in ranunculi, conifers, poplars, alders etc. may cause capillary damage leading to reddish discoloration of milk Feeding of moldy sweet clover (dicoumarin poisoning) may also cause bloody milk. Some leafy plants e.g. spurge (Euphorbia), sedge and shave grass contain a red dye which may appear in milk leading to its reddish discoloration. (Balhara et al., www.buffalopedia.cirb.res.in/).
Deficiency of blood platelets (thrombocytopenia): Cattle affected with diseases characterized by low platelet count may show reddish or pinkish discoloration of milk due to leakage of blood into milk (George et al., 2008). Normal platelet count in cow is 1-8×105 per µl. (Radostits et al., 2007).
Other causes: Other causes of bloody milk include vitamin C deficiency (Heidrich and Renk, 1967), rough milking and acute or chronic mastitis (Balhara et al., www.buffalopedia.cirb.res.in/)
Diagnostic workups
- Blood in milk is usually diagnosed on the basis of clinical If the milk with suspected presence of blood is left undisturbed for a few hours in a transparent glass container, the lower portion of the milk in that container will reveal the presence of blood clots when hemorrhage is the cause of bloody milk. No sedimentation of RBCs will occur when reddish discolouration is due to lysis of RBCs and colour of milk will remain uniform throughout (George et al., 2008). Centrifugation of milk at a speed of 2500 rpm for 10 minutes will result in visible sedimentation of RBCs at the bottom of a centrifuge tube made up of transparent glass. In cases in which the presence of extremely little blood in milk is suspected, benzidine test or Hemoccult slide test (Smith-Kline Diagnostics) can be performed to confirm the presence of blood in milk. It should be remembered that benzidine is a known carcinogen and as such its use should be avoided.
- Perform blood platelet count in cases which do not respond to conventional treatment as thrombocytopenia is one of the causes of blood in milk (George et al., 2008)
- Perform surf field mastitis test (Muhammad et al., 2010) to rule out mastitis as a cause of blood in milk. To this end, mix an equal quantity of 3% solution of house hold detergent (i.e. Surf Excel) and milk sample of each quarter The formation of gel indicates the presence of mastitis.
- Centrifugation of fresh milk to determine whether the reddish discoloration of milk is due to intact RBCs (associated with hemorrhage in the udder) or due to lysed RBCs (associated with leptospirosis and other systemic microbial infections or due to red dye in the leaves of fodder). If centrifugation facility is not available, let a sample of milk stand undisturbed for several hours in a transparent container and then look for sedimentation of RBCs at the bottom of the container. The formation of a bead of RBCs at the bottom of the centrifugation tube indicates hemorrhage.
Treatment: Different treatment strategies available for the treatment of blood in milk have been briefly described below:
- Intravenous administration of calcium: Intravenous injection of 300-450ml of calcium borogluconate plus magnesium and phosphorus is the standard treatment (Radostits et al., 2007). Treatment may have to be repeated daily for 2-3 days. Calcium has a coagulant property.
- Parenteral coagulants: According to Radostits et al. (2007), injections of coagulants are likely to give better cure rates than calcium Inj. AnaroxylR (Adrenochrome monosemicarbazone, 5 mg/ml; 8-10 injections for a cow or buffalo) or Inj. TransamineR (Tranexamic acid, 500 mg/ml; 10-15ml intramuscularly for a cow or buffalo; Muhammad et al., 1997) can be used to treat a cow/buffalo suffering from blood in milk. However, according to Eddy and Clark (1982) and Ayaz (1999), injectable coagulants are not effective in the treatment of blood in milk in cows and buffaloes.
- Local coagulants: Hungerford (1990) recommends intramammary infusion of coagulants e.g. Inj. ThrombonarR or Inj. ThrombostatR A strong solution say 2000 units/ml can be made, the affected quarter milked out and the material infused intramammary for a local coagulant effect. This should be done only in severe cases of blood in milk.
- Local and parenteral vasoconstrictors: It is well known that the circulatory system of the udder is very sensitive to the vasoconstrictor action of (Heidirch and Renk, 1967).That is why adrenaline is indicated in the treatment of bloody milk. Five to 8 ml of adrenaline (1:1000) can be injected subcutaneously to treat blood in milk in cows and buffaloes. As an alternative, 5ml of adrenaline can be mixed with 20 ml of normal saline and the solution infused into the teat producing milk with reddish discoloration. Ergot alkaloids e.g. ergonovine maleate (ErgometrineR), methylergometrine hydrogen maleate (MethergineR), ergotamine tartrate and dihydroergotamine have a variable degree of vasoconstrictor effect and thus can be used in the treatment of blood in milk when this condition is due to hemorrhage from a small blood vessel in the udder or teat. The dosages of different ergot alkaloids for large animals (horse, cow and buffalo) are as below:
Ergonovine maleate (ErgometrineR) = 10-20mg Methylergometrine hydrogen maleate (Inj. MethergineR, each 1 ml ampoule contains 0.2mg of methylergometrine hydrogen maleate) = 10-12 ampoules intramuscularly for a cow or buffalo.
Inj. SergotonineR is a proprietary preparation marketed by Rhone Merieux, France. Each 100ml of this injection contains double sulphate of 5-hydroxytryptamine and creatinine (0.25g), ergometrine maleate (0.02g) and isotonic saline solution q.s. to 100ml. The dose of this preparation is 3 to 4ml per 100kg b.wt. intramuscularly in cows, buffaloes and mares which can be repeated after 48hours,
- Administration of vitamin C: Dissolve 30 tablets of CeconR ,each tablet contains 500 mg of vitamin C) in 500 ml of ordinary water and give this solution as a drench. Poustin-CR is a polyethoxylated vitamin-C (a stable form of vitamin C) which can be used as an alternative of tablet CeconR. It is important to remember that hypervitaminosis C is not generally harmful in the Rather it is beneficial.
- Administration of antioxidants: The cows and buffaloes which are suffering from blood in milk can be treated with the following recipe: Dissolve 15 sachets of MucolatorR (Acetylcysteine; 200mg per sachet;) in 500 ml of distilled or mineral water (e.g. Pure LifeR, Nestle). Filter this solution through 4 layers of muslin cloth (‘Mulmal ka kuprra’ in Urdu). Add this filtered solution to one liter of warm dextrose 5% solution and inject intravenously. The prepared solution should be at body temperature when given intravenously. After 30 minutes, administer 30 tablets of vitamin C (e.g. Tab. CeconR, Abbot Lab.) in the form of a drench. Repeat intravenous administration of MucolatorR and oral administration of Tab. CeconR for next 2 to 3 days .
- Oral/injectable camphor: Raval et al. (1998) studied the efficacy of camphor (Camphora officinarum; ‘Mushak Kafoor’ in Hindi) in buffaloes suffering from blood tinged milk. Camphor contains volatile acid, which has a styptic action. Twenty one buffaloes with clinical cases of blood tinged or bloody milk were treated with camphor in banana orally at a dose of two tablets twice a day. Before and after the camphor therapy, the milk samples of these animals were tested for the presence of blood, clinically as well as for occult blood with a strip cup and benzidine test in the laboratory. Affected animals recovered within three to five days. Camphor can probably be more effectively given in an injectable form e. 30-60 ml of camphorated oil into the pectoral muscle (Udall, 1954). This camphorated oil can be formulated by mixing 20 parts of camphor powder (finely ground) in 80 parts of olive oil). Cotton seed oil may be substituted for olive oil in this prescription. To make a preparation that will not become cloudy when cold, set the oil in a refrigerator for 2 or 3 days and filter while cold (Milks, 1946).
- Antibiotics: If the cause of blood in milk is not known, antibiotics should be given by injection as well as through intramammary route (Hungerford, 1990) Inj. LincospiraR seem to be good antibiotic preparations because of their lincomycin and spiramycin content which penetrate extremely well into the udder. When leptospiral mastitis (cold mastitis with no inflammation) is the cause of bloody milk, it may be treated by streptomycin (25mg /kg wt. intramuscular for 3-5 days).
- Blood transfusion: Transfusion of 4-6 liters of blood from a healthy donor should be considered when thrombocytopenia and other coagulation defects are suspected as the cause of blood in milk (George et al., 2008). The disease which has caused thrombocytopenia should be treated according to its
- Homeopathic treatment: Indian workers (Varsheny and Naresh, 2004) treated a total of 102 mastitic quarters (fibrosed, n= 40; nonfibrosed, n=62) and five cases each of blood in milk and udder edema in lactating buffaloes with a homeopathic complex consisting of Phytolacca 200c, Calcarea fluorica 200c, Silicea 30c, Belladona 30c, Bryonia 30c, Arnica 30c, Conium 30c and Ipecacuanaha Dose of this complex was 10 pills four times daily until recovery. Treatment was 80 and 96.72% effective in cases of fibrotic mastitis and nonfibrosed mastitis, respectively. Recovery period was 21-42 days (fibrosed) and 4-15 days (nonfibrosed). Buffaloes suffering from udder edema and blood in milk recovered in 2-5 days. The cost of treatment was US $ 0.07 per day. These investigators ascribed the effectiveness of this commercial homeopathic preparation in the treatment of fibrosed/nonfibrosed mastitis, udder edema and blood in milk to anti- inflammatory effect of Phytolocca on glandular and fibrous tissue, analgesic effects of Bryonia, absorptive effect of Silicea on fibrotic and scar tissue, anti-inflammatory effect of Belladona, antihemorrhagic and antiseptic effect of Arnica, local decongestive effect of Ipecacuanha and Calcarea fluorica.
- Ethnoveterinary treatment practices: A widely touted ethnoveterinary practice for treatment of cows/buffaloes consist of dissolving 250 grams of turmeric (‘Halthee’ in Hindi) powder in one liter of warm milk, addition of 250 grams of ‘sambaloo’ leaves and giving as a drench for 2-3 days. Many farmers resort to oral administration of a cake of Lifebuoy soap dissolved in half to one liter of milk for 2-3 This soap is not likely to be toxic because lactating cows are normally fed sponified fat (= soap e.g. MegalacR) to increase milk yield.
- Vaccination against leptospirosis: When several cows or buffaloes in a herd suffer from blood in milk and do not respond to antibiotics, and other treatment measures, the herd should be vaccinated against leptospirosis (Hungerford, 1990). A vaccine that contains several strains of leptospira along with other organisms is now commercially available in
- Ancillary and supportive treatment: Tape the end of normal quarters and allow the calf to suckle milk from the teat having blood in milk. Calves do not care about blood in milk. Do not allow an affected cow/buffalo to run. Rather keep her tethered as running will aggravate the condition. Application of ice cold water or crushed ice (placed in a cloth suspensory the 4 ends of which are tied at the back of the affected animal) helps in control of hemorrhage through vasoconstriction. The affected animals should be tethered with sand as the bedding material which should be hosed with cold water 3-4 times in a When the animal suffering from blood in milk sits on cold sand, this leads to vasoconstriction and control of hemorrhage in the udder or teat. George et al. (2008) recommends that the affected teat be milked only once a day. If this approach does not work after several days, milking of affected quarter should be totally stopped. It should be remembered that total stoppage of milking may cause formation of severe clots in the teat. Thorough cleanliness in the animal shed and on the dairy farm should be instituted as squalid managemental condition predispose to blood in milk. The feed or fodder which is suspected for causing blood in milk should be changed.
NB: More than one treatment measures (given above) may need to be instituted. Many cases of blood in milk take several days to respond to treatment.
References
Balhara, A.K., N. Rana, S.K. Phulia, and Suneshy. Blood in milk –causes and control. Accessed at www.buffalopedia.cirb.res.in/Barragry, T.B., 1994. Bovine mastitis. In: Veterinary Drug Therapy. Lea and Fabiger, Philadelphia, USA. pp: 655-688.