One World, One Health: Prevent Zoonoses, Stop the Spread
Kaushik Satyaprakash1# and Annada Das2
1Assistant Professor, Department of Veterinary Public Health and Epidemiology, Faculty of Veterinary and Animal Sciences, RGSC, Banaras Hindu University, Barkachha, Mirzapur, Uttar Pradesh-231001
2PhD Scholar, Department of Livestock Products Technology, Faculty of Veterinary and Animal Sciences, WBUAFS, Kolkata, West Bengal- 700037
#Corresponding Author: Kaushik Satyaprakash
e-mail id: kaushik_vph@bhu.ac.in
Introduction
In an interconnected world, where borders blur and ecosystems intertwine, the health of humans, animals and the environment are inextricably linked. The concept of ‘One Health’ recognizes this interdependence and advocates for a holistic approach to safeguarding global well-being. At its core lies the urgent need to prevent zoonotic diseases- those that leap from animals to humans or vice-versa- before they escalate into pandemics.
Zoonoses have shaped human history, from the Black Death to the more recent COVID-19 pandemic. These diseases emerge when pathogens- viruses, bacteria, or parasites- cross species barrier. Whether it’s a bat harbouring a novel coronavirus or a mosquito transmitting malaria, zoonoses remind us that our fate is intertwined with that of the animal kingdom.
The recent COVID-19 pandemic, as well as avian influenza and Ebola, is a stark reminder of how a disease originating in animals can have a global impact on human health and societies as a whole. In fact, one of the most recent Ebola virus outbreaks (the largest and most complex Ebola outbreak since 1976) affected over 28600 cases from 2014-16 in West Africa, with additional cases reported in other countries (Italy, Spain, the United Kingdom, and the United States). Meanwhile, the H5N1 bird flu has been extensively detected in the U.S., with 9253 wild birds and 90,604,876 poultry testing positive in the latest annual survey, posing a serious risk to human health. The transmission dynamics of such diseases are often multifaceted: increased urbanization pushes humans into previously unpopulated areas, climate change alters the habitats of disease carrying species, and global travel and trade facilitate the rapid spread of pathogens. In particular, around 75% of emerging infectious human diseases have an animal origin. In 2022, the most frequently reported zoonotic diseases in humans with the European Union were campylobacteriosis, with 137,000 cases, and salmonellosis, with 65,000 cases. Yersiniosis was the third most reported zoonosis, followed by infections caused by Shiga toxin-producing Escherichia coli and Listeria monocytogenes.
Cavin W. Schwabe, the father of Modern Veterinary Epidemiology, is often credited for the rebirth of the modern “One Medicine movement” and strongly advocated for collaboration between human and veterinary public health professionals to address zoonotic diseases. That ‘One Medicine’ has evolved into ‘One Health’ where emphasis has been given to health promotion rather than treating the diseases. Since then, the ‘One Health’ approach has transcended from traditional silos. It is an integrated framework that calls for collaborative action across various sectors, including public health, veterinary medicine, environmental science, and agriculture. Their collective mission is to detect, prevent, and respond to zoonotic threats swiftly and effectively. By strengthening surveillance systems, promoting responsible antibiotic use, and preserving wildlife habitats, we can break the chain of transmission.
Preventing zoonoses requires robust surveillance systems to detect threats early, encompassing disease tracking in humans, animals, and environmental changes. Early detection and response are critical to containing outbreaks before they escalate. Vaccination programmes for both animals and humans, alongside accessible treatments, from essential parts of this strategy.
Biosecurity measures are vital in preventing pathogen spread, involving strict protocols in agriculture, wildlife trade, and food markets to minimize cross-species transmissions. Public education campaigns are crucial for raising awareness about zoonotic risks and promoting behaviours that reduce these risks.
In this context, food traceability plays a pivotal role in the control and prevention of infectious diseases transmitted through the food supply. In the broader context of public health, food traceability is not just a tool for crisis management but a foundational aspect of preventive health policies, helping to mitigate the risk of large-scale foodborne outbreaks and enhancing the overall safety of the food supply. The critical importance of these systems was starkly highlighted by the mad cow disease.
Stopping zoonotic disease spread demands cross-sector collaboration and strong policy frameworks. Research and innovation are pivotal, providing the tools and knowledge to tackle zoonotic threats. Investing in scientific research to understand these diseases, develop diagnostics, and create vaccines and treatments is imperative. Therefore, ‘One world, One health’ represents a paradigm shift in addressing global health challenges. By recognizing the interconnectedness of human, animal, and environmental health and fostering cross-disciplinary collaboration, we can create resilient systems to prevent and control zoonotic diseases, ensuring a healthier, more sustainable world.
Understanding ‘Zoonoses’
The joint WHO/FAO Expert Group on Zoonoses defined ‘zoonoses’ as ‘those diseases and infections which are naturally transmitted between vertebrate animals and man” (WHO, 1978). The term ‘Zoonoses’ was coined by Rudolf Virchow. In a scoping review it has been mentioned that, out of the 1407 recognized species as human pathogens, around 816 (nearly 58%) are zoonotic in nature. As many as 177 (13%) of the total pathogens are regarded as emerging or reemerging, and of these, 130 (75%) were classified as zoonoses (Woolhouse et al., 2005). Understanding these diseases involves recognizing the epidemiology, risk factors, transmission pathways along with implementing measures like surveillance, early detection, and public education to prevent the outbreaks. The ‘One Health’ approach, integrating efforts across health sectors, is essential for effective management and control
Understanding the ‘One Health’ Approach
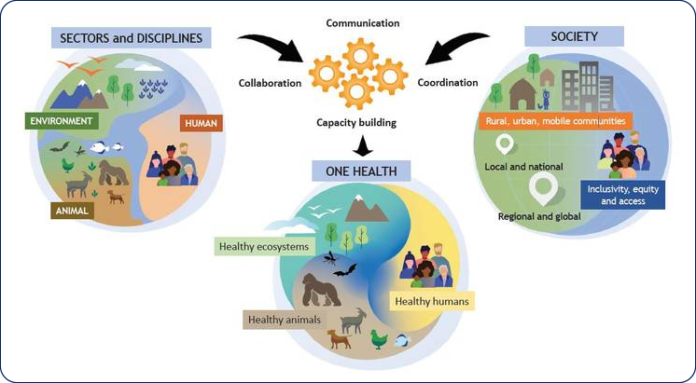
Recognizing the urgency and complexity surrounding ‘One Health’ and in order to drive this concept forward into policies and actions, four international organizations, namely, the Food and Agriculture Organization (FAO) of the United Nations, the World Organization for Animal Health (OIE), the World Health Organization (WHO) and the United Nations Environment Programme (UNEP) joined hands together to establish the interdisciplinary “One Health High-Level Expert Panel” (OHHLEP) in May 2021. The OHHLEP gave the working definition of ‘One Health’ which revolve around the practical implementation of the 4 ‘C’s: Communication, Coordination, Collaboration, and Capacity building (fig. 1).
“One Health is an integrated, unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems. It recognizes the health of humans, domestic and wild animals, plants, and the wider environment (including ecosystems) are closely linked and interdependent.” The approach mobilizes multiple sectors, disciplines and communities at varying levels of society to work together to foster well-being and tackle threats to health and ecosystems, while addressing the collective need for clean water, energy and air, safe and nutritious food, taking action on climate changes and contributing to sustainable development (OHHLEP, 2021).
Fig. 1 The ‘One Health’ Approach developed by the OHHLEP
These are based on several fundamental principles, including equity (between sectors and disciplines), parity (sociopolitical and multicultural), socioecological equilibrium (harmonious balance between human-animal-environment interaction), stewardship and responsibility of humans to adopt sustainable solutions, and trans-disciplinarity and multisectoral collaboration with relevant disciplines. The collaboration across sectors and disciplines contributes to protect health, address various public health issues, including the emergence of zoonotic diseases, antimicrobial resistance, and food safety. By interlinking various domains of human health, animal health and environmental health, the ‘One Health’ can help to address the full spectrum of zoonotic disease control- from diagnosis to prevention, preparedness, response and management- and contribute to global health security. The One Health paradigm forges co-equal, all-inclusive collaborations between animal, plant, environmental and human health arenas, i.e. chemical, engineering and social scientists, dentists, nurses, agricultural/ horticulturalists and food producers, wildlife and environmental health specialists and many other related disciplines that fall under its purview.
Challenges and trends in zoonotic disease
The emergence of zoonotic disease is influenced by several interconnected trends, demanding our attention and action:
- Increased demand for animal protein:
- As global populations grow, so does the demand for meat, milk and other animal products.
- Intensive animal farming and wildlife trade create ideal conditions for zoonotic spillover
- The close proximity of humans, livestock, and wildlife facilitates pathogen transmission
- Unsustainable farming practice:
- Factory farming, overcrowded conditions, and suboptimal hygiene increase disease risk.
- Antibiotic use in agriculture contributes to antimicrobial resistance.
- Encroachment into natural habitats disrupts ecosystems and exposes humans to novel pathogens.
- Climate change and ecological shifts:
- Altered ecosystems due to climate change affect animal behaviour and migration patterns
- Vector-borne diseases (e.g. Lyme disease, Zika) expand their range.
- Melting ice exposes ancient pathogens from permafrost.
- Urbanization and wildlife interface:
- Urban sprawl encroaches on wildlife habitats, leading to human-wildlife interactions.
- Bats, rodents, and other reservoir species can transmit viruses to humans
- Global travel and trade:
- Rapid movement of people and goods facilitate pathogen spread.
- Air travel can turn a local outbreak into a global pandemic within days.
- Human behaviour and cultural factors
Challenges for managing zoonotic diseases
Some of the major challenges for managing zoonotic diseases include,
- Insufficient information on the burden, trend and risk of zoonotic diseases
- Poor awareness among policy makers
- Inadequate resources and skilled manpower
- Inadequate collaboration and partnership across sectors
- Lack of integration between human and veterinary sectors for exchange of epidemiological and laboratory surveillance data
- Weak disease surveillance system
- Inadequate diagnostic facilities
- Inadequate community participation
- Poor application of control measures in health-care facilities
- Inappropriate or inadequate vector control strategies
Stopping the spread- Strategies to prevent and control zoonotic diseases
Practically, no universal strategy exists for prevention and control of emerging zoonotic diseases may be due to the lack of coherence between animal and human health sector in many parts of the world. Efforts were undertaken at regional levels to curb the spread during outbreaks of various zoonotic diseases. Considering the magnitude of the problem and the ever-increasing public health risks associated with zoonotic diseases, now it’s the time perhaps, for a paradigm shift to address the global threats.
- Effective collaboration between animal and human health sector
- Regular exchange of scientific information
- Creation of joint task forces
- Joint field investigations and sharing institutional resources within a coordinated framework
- Surveillance and early detection
- Establish robust surveillance to monitor animal and human health
- Integration of disease surveillance system between the animal and human health sectors
- Use of syndromic surveillance system for real-time detection of the threats
- Strengthening laboratory diagnostic capabilities for novel pathogens
- Creation of state-of-the art laboratories and upgradation of existing laboratories
- Skill upgradation and training of the personnel
- Increasing funding for research and diagnosis
- Integrated vector control management approach
- Vector control measures including rodents
- Setting up of sentinel sites for entomological surveillance
- Improved hygiene and sanitation
- Promote proper hygiene practices in communities, farms, and wildlife habitats.
- Ensure safe handling of animal products and waste.
- Responsible antimicrobial usage
- Community education on prudent antimicrobial usage
- Adherence to prescribed treatments and avoiding self-medication
- Controlling the sake of antibiotics to prevent over-the-counter purchase without prescription
- Antimicrobial sensitivity testing wherever possible before drug administration
- Wildlife conservation:
- Protect natural habitat and biodiversity
- Reduce human-wildlife interaction to minimize disease transmission.
- Education and awareness:
- Educate public about zoonotic diseases and the associated risks
- Encourage community participation in disease transmission
- Research and innovation:
- Investing in research to understand zoonotic diseases and develop new diagnostic tools, treatments and vaccines
- Encouraging innovations in surveillance technology and data analysis
- Behavioural aspect of zoonotic diseases for safe handling of animals by humans
- Environmental protection:
- Preserving natural habitats and biodiversity to reduce human-wildlife interaction that can lead to a zoonotic spillover
- Implementing sustainable agricultural practices
- Developing epidemic preparedness and response capacities for emerging zoonoses
- Developing national plan involving all important stakeholders
- Strengthening human, animal and vector surveillance, data should be integrated and shared
- Development of appropriate guidelines and standards to measure the effectiveness of response operations
- Setting up a multi-disciplinary coordinating body to foster collaboration and integration among all partners
- Policy and Legislation:
- Developing and enforcing policies that support ‘One Health’ concept
- Ensuring that international regulations and agreements promote global health security
- National capacity building and promoting research
- Health education, risk communication and social mobilization
By implementing these strategies, we can create a healthier, safer world for both humans and animals.
‘One Health’ approach for control of Zoonotic Tuberculosis- the first of its kind
In the context of the Sustainable Development Goals (SGDs), the WHO’s End TB strategy recognizes the diagnosis and treatment of each and every human TB cases. Although, Mycobacterium tuberculosis is the chief architect of TB in humans, a significant proportion of human TB cases is attributable to the infection caused by Mycobacterium bovis, a member of the M. tuberculosis complex. Within animal population, M. bovis is the causative agent of bovine TB. Human beings can acquire M. bovis from animals through contaminated food (milk, meat or products thereof) as well as through airborne transmission leading to the establishment of zoonotic TB infection, which often establishes in extra-pulmonary sites in humans. The true burden of zoonotic TB is very much underestimated due to lack of routine surveillance data and inefficient laboratory procedure to differentiate between M. tuberculosis and M. bovis. In order to achieve the WHO’s End TB strategy, it is of utmost importance to diagnose and treat the people affected with zoonotic TB. Again, zoonotic TB in people can’t be addressed without controlling bovine TB and improving food safety which can only be possible though a ‘One Health’ approach. Recognizing the interdependence of human and animal health sectors to address the major health and economic implication of this disease, a ‘Zoonotic TB Control Roadmap’ has been prepared for the first time jointly by the WHO, OIE, FAO and the International Union Against Tuberculosis and Lung Disease (The Union) in October 2017. This roadmap is centred around the ‘One Health’ approach in which 10 priority areas of action to control zoonotic TB are enlisted. This roadmap can also be applied for the control of other zoonotic and foodborne diseases. These are as follows:
- Improve the Scientific Evidence Base
- Systematically survey, collect, analyse and report better quality data on the incidence of zoonotic TB in people, and improve surveillance and reporting of bovine TB in livestock and wildlife
- Expand the availability of appropriate diagnostic tools and capacity for testing to identify and characterize zoonotic TB in people
- Identify and address research gaps in zoonotic and bovine TB, including epidemiology, diagnostic tools, vaccines, effective patient treatment regimens, health systems and interventions coordinated with veterinary services.
- Reduce Transmission at Animal-Human Interface
- Develop strategies to improve food safety.
- Develop capacity of the animal health sector to reduce the prevalence of TB in livestock.
- Identify key populations and risk pathways for transmission of zoonotic TB
- Strengthen Intersectoral and Collaborative Approaches
- Increase awareness of zoonotic TB, engage key public and private stakeholders and establish effective intersectoral collaboration.
- Develop and implement policies and guidelines for the prevention, surveillance, diagnosis, and treatment of zoonotic TB, in line with intergovernmental standards where relevant
- Identify opportunities for community-tailored interventions that jointly address human and animal health
- Develop an investment case to advocate for political commitment and funding to address zoonotic TB across sectors at the global, regional and national levels.
Conclusion
Rudolf Virchow, the father of modern pathology and comparative medicine has aptly stated in 1885 that “Between animal and human medicines, there are no dividing lines, nor there should be. The object is different but the experience obtained constitutes the basis of all medicine”. The ‘One Health’ approach is essential for preventing zoonoses and halting their spread. By recognizing the interconnectedness of humans, animals, and environmental health, this holistic strategy fosters cross-sector collaboration, early detection, and comprehensive disease management. Implementing robust surveillance, biosecurity measures, and public education can significantly reduce zoonotic disease risks. Investing in research and innovation further strengthens our defence against future outbreaks. Ultimately, adopting the ‘One Health’ approach ensures a resilient, sustainable global health system, safeguarding the well being of all species and promoting a healthier and, more secure world.
References
- Ahmed, S.; Dávila, J.D.; Allen, A.; Haklay, M.M.; Tacoli, C.; Fèvre, E.M. Does urbanization make emergence of zoonosis more likely? Evidence, myths and gaps. Urban.2019, 31, 443–460.
- Esposito, M.M.; Turku, S.; Lehrfield, L.; Shoman, A. The Impact of Human Activities on Zoonotic Infection Transmissions. Animals2023, 13, 1646.
- Islam, A.; Ferdous, J.; Islam, S.; Sayeed, M.A.; Dutta Choudhury, S.; Saha, O.; Hassan, M.M.; Shirin, T. Evolutionary Dynamics and Epidemiology of Endemic and Emerging Coronaviruses in Humans, Domestic Animals, and Wildlife. Viruses2021, 13, 1908.
- Jato-Espino, D.; Mayor-Vitoria, F.; Moscardó, V.; Capra-Ribeiro, F.; Bartolomé Del Pino, L.E. Toward One Health: A spatial indicator system to model the facilitation of the spread of zoonotic diseases. Public Health2023, 11, 1215574.
- Ryu, W.S. New Emerging Viruses. In Molecular Virology of Human Pathogenic Viruses; Academic Press: Cambridge, MA, USA, 2017; pp. 289–302.
- WHO/FAO. WHO Expert Committee on Parasitic Zoonoses & World Health Organization. Parasitic Zoonoses: Report of a WHO Expert Committee, With the Participation of FAO [meeting held in Geneva from 14 to 20 November 1978]. World Health Organization. (1979). Available online at: https://apps.who.int/iris/handle/10665/41353
- Woolhouse, M. E., & Gowtage-Sequeria, S. (2005). Host range and emerging and reemerging pathogens. Emerging infectious diseases, 11(12), 1842–1847. https://doi.org/10.3201/eid1112.050997