ONE HEALTH APPROACH IN PREVENTING ZOONOTIC DISEASES FOR A HEALTHY WORLD
Anubhab Aditya and Kautuk Kumar Sardar
College of Veterinary Science & Animal Husbandry,
Odisha University of Agriculture & Technology,
Bhubaneswar -751 003, Odisha
Abstract
The concept of One Health has emerged as a pivotal framework for addressing global health challenges, particularly in the context of zoonotic diseases, those transmitted between animals and humans. This article explores the interrelationship between human, animal, and environmental health within the One Health paradigm. It offers a comprehensive analysis of zoonotic disease dynamics, examining key examples such as Avian influenza, Brucellosis, Ebola virus disease, COVID-19, Lyme disease, and Rabies. This article also investigates the multifaceted factors contributing to zoonotic disease emergence and transmission, discusses strategies for prevention and control, global initiatives, challenges, and outlines future directions in the field of One Health.
Key words: Zoonotic diseases, One health, Prevention, Control, Transmission.
Introduction
Zoonosis, an infectious disease, has jumped from a non-human animal to humans and vice-versa (WHO). They encompass a wide range of pathogens, including bacteria, viruses, parasites, and fungi. According to the World Health Organization (WHO), 60% of all infectious diseases and 75% of emerging infectious diseases are zoonotic (WHO, 2020). The compass of zoonoses extends from common infections like Salmonella to arising pitfalls like Ebola and SARS- CoV- 2. Zoonotic conditions have profound significance for public health, animal health, and ecological balance. The adding frequencies of zoonotic outbreaks underscores the necessity for effective forestalment and control measures. Factors similar as urbanization, deforestation, and global trip contribute to the spread and emergence of zoonotic conditions, making it pivotal to borrow a holistic approach to complaint forestalment. The interdependence of human, animal, and environmental health underscores the critical need for intertwined approaches to global health challenges. One Health represents such an approach, emphasizing collaboration across disciplines to achieve optimal health issues for all. Understanding the dynamics of zoonotic complaint transmission and enforcing effective forestalment and control measures are imperative to guard human and animal populations. The One Health conception integrates humans, animal, and environmental health into a unified approach to complaint forestalment and control. This frame advocates for interdisciplinary collaboration among veterinarians, croakers, environmental scientists, and policymakers to address health issues exhaustively. One Health emphasizes that the health of humans, creatures, and the terrain are connected, and results bear common problems across these disciplines. There’s a dire need to inculcate current knowledge on zoonotic conditions within the environment of One Health, furnishing perceptivity into strategies for mollifying these global health pitfalls.
Origin and Historical background:
The 1918 influenza pandemic, caused by the H1N1 influenza virus, remains one of the most catastrophic global health crises in history. Originating from avian influenza viruses, the pandemic led to the death of approximately 50 million people worldwide (Taubenberger & Morens, 2006). The pandemic illustrated the potential of zoonotic diseases to cause widespread mortality and highlighted the need for improved surveillance and response strategies.
The Severe Acute Respiratory Syndrome (SARS), caused by the SARS-CoV virus, emerged in 2003 and rapidly spread across Asia and beyond. Originating in bats and transmitted to humans through civet cats, the outbreak affected over 8,000 individuals and resulted in nearly 800 deaths (Peiris et al., 2004). The SARS outbreak emphasized the importance of understanding zoonotic transmission pathways and the necessity for international cooperation in outbreak response.
The Ebola virus epidemic in West Africa, which began in 2014, was caused by the Ebola virus, with bats as the likely reservoir. The epidemic resulted in over 11,000 deaths and revealed significant gaps in global health infrastructure and response capabilities (WHO, 2016). The outbreak underscored the importance of rapid detection, containment, and the role of effective communication in managing zoonotic crises.
Quite recently, the COVID-19 Pandemic, a zoonotic disease, originated in animals before jumping to humans. SARS-CoV-2, the virus causing COVID-19, is believed to have emerged from bats, which are known carriers of various coronaviruses. The exact pathway of transmission to humans remains under investigation, but it is suspected that the virus may have passed through an intermediary host species, possibly a wild animal sold at a seafood market in Wuhan, China. This zoonotic spillover is an example of how viruses can cross species barriers, facilitated by factors such as close contact between wildlife and humans, habitat destruction, and wildlife trade.
Threat of Zoonotic Diseases:
Zoonotic conditions are caused by pathogens that naturally infect both creatures and humans. These pathogens include contagions, bacteria, spongers, and fungi, able of crossing species walls through direct contact, consumption of defiled food or water, or exposure to infected vectors. The global impact of zoonoses is illustrated by recent outbreaks similar as COVID- 19, which has led to a ruinous epidemic with profound health, social, and profitable consequences. Other notable exemplifications include Ebola contagion complaint, known for its high mortality rates and epidemic eventuality; colourful strains of avian influenza hanging both animal and human populations; and rabies, continuing to beget significant mortal morbidity and mortality in regions with shy healthcare structure. Mortal conditioning similar as deforestation, urbanization, and artificial husbandry have altered ecosystems and increased mortal- beast relations. These changes contribute to the emergence and re-emergence of zoonotic conditions. The concept of “disease emergence” refers to the appearance of new or previously known diseases in new regions or populations, often driven by environmental and socio-economic factors (Jones et al., 2008).
Understanding the factors contributing to the emergence and transmission of zoonotic conditions is essential for developing effective forestalment and control strategies. These conditions frequently appear in wildlife populations and can unmask over into mortal populations through colourful pathways. Environmental changes, including deforestation, urbanization, and climate change, alter ecosystems and bring humans into near contact with wildlife, adding the threat of zoonotic spill over events.
Factors Contributing to Zoonoses
Several interconnected factors contribute to the emergence, transmission, and spread of zoonotic diseases:
- Environmental Changes: Anthropogenic conditioning similar as deforestation, urbanization, and climate change alter ecosystems, leading to niche loss and fragmentation. These changes can bring humans into near contact with wildlife budgets of contagious agents, adding the threat of spill over events.
- Intensive Agriculture and Wildlife Trade: Practices similar as ferocious husbandry, wildlife trafficking, and bush meat consumption produce surroundings where zoonotic pathogens can thrive and broadcast among beast populations. near propinquity between wildlife, beast, and humans in these settings facilitates complaint transmission.
- Globalization and Travel: Increased global Trip and trade contribute to the rapid-fire spread of pathogens across geographical boundaries. Infected individualities or creatures can serve as vectors, introducing pathogens into new surroundings and populations, thereby amplifying the eventuality for complaint outbreaks.
Understanding these complex interactions is essential for developing targeted interventions aimed at reducing the risk of zoonotic spillover events and mitigating the impact of emerging infectious diseases on human and animal health.
Major Zoonotic Diseases
The zoonotic diseases are classified as-
Bacterial Zoonoses:
- Salmonellosis– Salmonellaspecies are a leading cause of foodborne illness worldwide. The bacteria can be transmitted through contaminated food, water, and contact with infected animals. Effective control measures include proper food handling, sanitation, and vaccination of livestock. Surveillance programs and public education campaigns play a crucial role in reducing the incidence of salmonella infections (CDC, 2021)
- Pathophysiology and symptoms show that Salmonella infections can cause symptoms ranging from mild gastroenteritis to severe systemic illness. Common symptoms include diarrhoea, fever, abdominal cramps, and vomiting. In severe cases, salmonella can lead to bloodstream infections and other complications.
- Prevention strategies for Salmonella include food safety. So, proper cooking and handling of food, particularly poultry and eggs be should be taken care. The hygiene practices include regular handwashing and sanitation of food preparation surfaces along with immunization of poultry and livestock to reduce the prevalence of salmonella.
- Lyme Disease:Lyme disease is caused by the bacterium Borrelia burgdorferi, transmitted to humans through the bite of infected black-legged ticks. The disease presents with symptoms such as fever, rash, and joint pain. Prevention includes tick avoidance, prompt removal of ticks, and use of protective clothing. Early diagnosis and treatment with antibiotics are crucial for preventing long-term complications (Wormser et al., 2006).
- Pathophysiology and symptoms of Lyme disease demonstrates that it progresses through three stages: early localized, early disseminated, and late disseminated. Early symptoms include erythema migrans (a characteristic “bull’s-eye” rash), flu-like symptoms, and fatigue. If untreated, the disease can lead to chronic symptoms such as arthritis, neurological complications, and heart problems.
- Prevention and Control: Prevention measures for Lyme disease include Tick Avoidance, using insect repellent, wearing protective clothing, and performing tick checks after outdoor activities, prompt tick removal as soon as possible to reduce the risk of disease transmission. There is an all time need to develop and use of vaccines to prevent Lyme disease in high-risk areas. To prevent of the disease.
- Brucellosis-: Brucellosis is another important zoonotic disease which caused by bacteria from the Brucella genus, affecting both humans and animals. It is transmitted through unpasteurized milk, undercooked meat, and direct contact with infected animals. Control strategies include vaccination of livestock and pasteurization of milk. Public health education and surveillance are essential for managing brucellosis (Corbel, 2006).
- Pathophysiology and symptoms: Brucellosis can cause a range of symptoms, including fever, sweats, malaise, and joint pain. Chronic infections can lead to more severe complications such as arthritis, endocarditis, and reproductive problems.
- Prevention and control strategies for brucellosis embraces immunization of livestock to prevent the spread of brucellosis. The food safety is a big concern pasteurization of milk and proper cooking of meat products; are utmost necessary including surveillance, monitoring and controlling outbreaks in animal populations.
- Leptospirosis: Leptospirosis is caused by bacteria of the genus It is transmitted through contact with contaminated water, soil, or animal urine. Symptoms range from mild flu-like illness to severe disease with liver and kidney damage. Preventive measures include avoiding contact with potentially contaminated environments and improving sanitation (Bharti et al., 2003).
- Looking at the pathophysiology and symptoms of leptospirosis, it embarks on the journey of symptoms such as fever, headache, muscle aches, and jaundice. It has been found that severe cases can lead to organ failure, bleeding, and respiratory distress leading to death of human beings.
- Prevention and control strategies for leptospirosis encompasses avoiding contaminated environments, reducing contact with water and soil contaminated with animal urine, improving sanitation, ensuring proper waste disposal and hygiene in areas prone to contamination. The educating at-risk public populations about preventive measures and symptoms of leptospirosis. Is of prime importance to contain the disease.
Viral Zoonoses
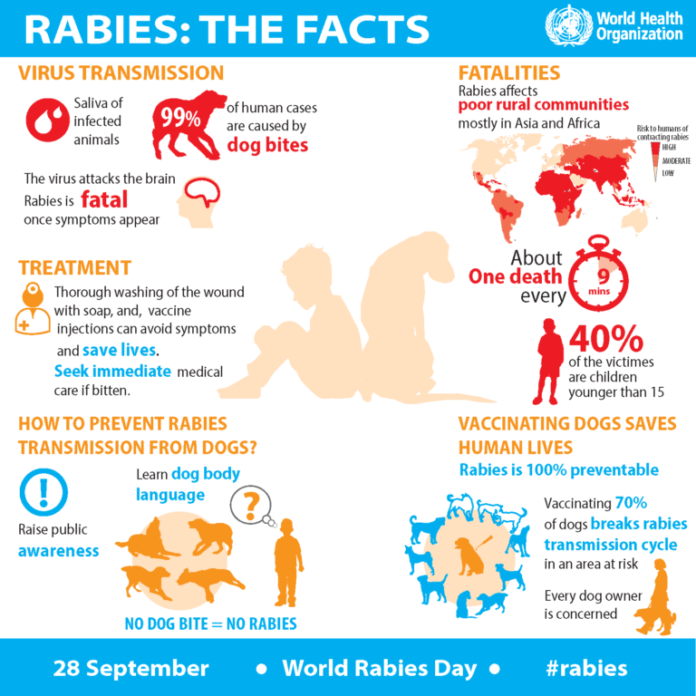
- Rabies: Rabies is a fatal viral disease which is transmitted through the bite of an infected animal, typically a dog. The rabies virus affects the central nervous system and is almost always fatal once clinical symptoms appear. The prevention involves vaccination of pets, post-exposure prophylaxis for exposed individuals, and public education (Jackson, 2003).
(Source-World Health Organization. Available at https://cdn.who.int/media/docs/default-source/searo/india/health-topic-pdf/rabies-infographic-updated-global-international-meeting.pdf?sfvrsn=6f9abb6d_2)
- Pathophysiology and Symptoms: Rabies progresses through several stages, including the prodromal stage, acute neurological phase, and coma. Initial symptoms include fever, headache, and malaise, followed by neurological symptoms such as agitation, confusion, and hydrophobia. Once symptoms appear, rabies is almost invariably fatal.
- Prevention and Control: Prevention strategies for rabies include: Vaccination: Immunization of pets and wildlife to reduce the risk of rabies transmission; Post-Exposure Prophylaxis: Administration of rabies vaccine and rabies immune globulin to individuals exposed to potentially rabid animals; Public Education: Raising awareness about rabies prevention and the importance of seeking medical care after potential exposure.
- Hantavirus: Hantavirus is transmitted to humans through contact with rodent droppings, urine, or saliva. It can cause hantavirus pulmonary syndrome (HPS) or haemorrhagic fever with renal syndrome (HFRS). Prevention focuses on reducing rodent exposure, proper cleaning techniques, and early detection of symptoms (Mills et al., 1999).
- Pathophysiology and Symptoms- Hantavirus infections can cause severe respiratory or renal symptoms. HPS is characterized by fever, muscle aches, and a sudden onset of respiratory distress, while HFRS presents with fever, bleeding, and kidney damage.
- Prevention and Control- Prevention measures for hantavirus include: Rodent Control: Implementing measures to reduce rodent populations and prevent contact with rodent excreta; Proper Cleaning: Using appropriate disinfectants and personal protective equipment when cleaning areas contaminated with rodent droppings; Early Detection: Monitoring for symptoms and seeking medical care promptly if exposure to rodents occurs.
Other Zoonoses
- Toxoplasmosis- Toxoplasmosis is caused by the protozoan parasite Toxoplasma gondii. It can be transmitted through consumption of undercooked meat, contaminated water, and contact with cat faeces. Most infections are asymptomatic, but severe cases can affect the eyes and brain. Preventive measures include proper food handling, hygiene practices, and avoiding contact with cat litter (Montoya & Liesenfeld, 2004).
- Pathophysiology and Symptoms- Toxoplasmosis can cause flu-like symptoms in healthy individuals but may lead to more severe complications in immunocompromised individuals and pregnant women. Congenital toxoplasmosis can result in severe outcomes, including vision and developmental problems in infants.
- Prevention and Control- Prevention strategies for toxoplasmosis include: Food Safety: Cooking meat to safe temperatures and washing fruits and vegetables; Hygiene Practices: Regular handwashing and avoiding contact with cat litter; Public Education: Informing at-risk populations about the importance of preventive measures.
- Cryptococcosis- Cryptococcosis is caused by the fungus Cryptococcus neoformans, which is found in soil and bird droppings. It primarily affects immunocompromised individuals and can cause severe respiratory and neurological symptoms. Prevention involves managing underlying conditions and avoiding exposure to environments with high levels of fungal spores (Perfect et al., 2010).
- Pathophysiology and Symptoms- Cryptococcosis can present as a pulmonary infection or disseminate to the central nervous system, leading to cryptococcal meningitis. Symptoms include cough, fever, headache, and neck stiffness.
- Prevention and Control- Prevention measures for cryptococcosis include: Managing Immunocompromised Conditions: Ensuring proper treatment and monitoring of individuals with compromised immune systems; Avoiding Exposure: Minimizing contact with environments that may be contaminated with fungal spores; Public Education: Raising awareness about the risks of cryptococcosis and preventive measures.
Understanding One Health
One Health is a holistic and interdisciplinary approach that recognizes the interconnections between human health, animal health, and environmental health. It acknowledges that dislocations in one sector can have cascading goods across others, emphasizing the significance of collaboration and participated responsibility among medical professionals, veterinarians, ecologists, policymakers, and other stakeholders. One Health aims to address complex health challenges more effectively and sustainably by integrating perceptivity and moxie from different fields. In the environment of zoonotic conditions, this approach is pivotal for understanding the ecological and epidemiological factors that contribute to complaint emergence, transmission, and continuity. The term gained elevation in the early 2000s, reflecting a paradigm shift towards a more intertwined and cooperative approach to address arising contagious conditions, particularly those of zoonotic origin. Zoonoses, conditions transmitted between creatures and humans, have historically posed significant pitfalls to public health, with outbreaks similar as Ebola, SARS, and avian influenza pressing the global impact of these connected health challenges. One World, One Health Concept
Origins and Development: The One Health concept emerged from the recognition that human, animal, and environmental health are intricately linked. It gained prominence in the early 2000s, with significant contributions from organizations such as the World Health Organization (WHO), the Food and Agriculture Organization (FAO), and the World Organisation for Animal Health (OIE). The 2004 International Conference on Emerging Infectious Diseases marked a pivotal moment in the formal endorsement of One Health principles (CDC, 2004).
- Core Principles: The core principles of One Health include:
- Interconnectedness: Recognizing that the health of humans, animals, and the environment are interlinked.
- Collaboration: Encouraging interdisciplinary collaboration to address complex health issues.
- Prevention and Control: Implementing integrated strategies to prevent and control zoonotic diseases.
Key Organizations and Initiatives:
- World Health Organization (WHO): The WHO plays a central role in global health, including the control of zoonotic diseases. It provides guidelines, conducts research, and facilitates international cooperation to address zoonotic threats (WHO, 2020). WHO’s initiatives include the Global Health Security Agenda and the Integrated Surveillance of Antimicrobial Resistance.
- Food and Agriculture Organization (FAO): The FAO focuses on animal health and food safety, promoting practices that prevent zoonotic disease transmission through agriculture and food production (FAO, 2018). The FAO’s initiatives include the monitoring of animal health, the promotion of safe food handling practices, and the development of guidelines for disease control.
- World Organisation for Animal Health (OIE): The OIE is responsible for improving animal health worldwide and provides standards and guidelines for the prevention and control of zoonotic diseases (OIE, 2019). The OIE’s initiatives include the development of international standards for animal health and the establishment of disease surveillance systems.
- Collaborative Efforts: Collaborative efforts include the Global Early Warning System for Major Animal Diseases and the One Health Joint Plan of Action, which bring together various stakeholders to tackle zoonotic diseases (One Health Initiative, 2020).
National policies and prevention strategies
In India, various policies and laws are in place to address and prevent zoonotic diseases. These regulations are designed to safeguard public health, animal health, and the environment. An overview of the key policies and laws relevant to preventing zoonoses in India are:
1.The Prevention of Cruelty to Animals Act, 1960
- Purpose: Primarily aimed at preventing cruelty to animals, this Act helps improve the welfare of animals, which can indirectly reduce the risk of zoonotic diseases by ensuring better living conditions. (India code website)
- Key Provisions: It covers the prevention of unnecessary pain and suffering, humane treatment, and welfare standards for animals.
- The Wildlife Protection Act, 1972
- Purpose: Regulates the protection of wildlife and their habitats, which is crucial in preventing zoonoses that can spread from wildlife to humans. (India code website)
- Key Provisions: Prohibits hunting and trade of protected wildlife species, regulates wildlife sanctuaries, and provides for the creation of protected areas.
- The Animal Diseases Act, 2001
- Purpose: Focuses on the control and prevention of animal diseases, which is essential for managing zoonotic threats. (India code website)
- Key Provisions: Provides for the notification of outbreaks of animal diseases, quarantine measures, and the establishment of disease-free zones.
- The National Animal Disease Reporting System (NADRS)
- Purpose: A surveillance system to monitor and report animal diseases, including zoonotic ones. (NADRS website)
- Key Features: Facilitates the collection and analysis of disease data, aiding in early detection and response to outbreaks.
5.The National Rabies Control Programme (NRCP)
- Purpose: Specifically addresses rabies, a major zoonotic disease in India. (NRCP website)
- Key Features: Includes vaccination of dogs, post-exposure prophylaxis for humans, and public awareness campaigns.
6.The National Health Mission (NHM)
- Purpose: Aims to improve public health, including aspects related to zoonotic diseases. (NHM website).
- Key Features: Supports health infrastructure, disease control programs, and preventive healthcare measures at the community level.
7.The Food Safety and Standards Act, 2006
- Purpose: Regulates food safety and standards, which include controls on the handling and processing of animal products to prevent zoonotic infections. (India Code website)
- Key Provisions: Establishes standards for food safety, including hygiene practices in meat and dairy processing.
8.The Biosecurity Guidelines for Livestock and Poultry
- Purpose: Provides guidelines to prevent the spread of diseases among livestock and poultry, many of which are zoonotic. (DAHD website)
- Key Features: Includes biosecurity measures such as quarantine protocols, sanitation practices, and disease surveillance.
9.The Plantations Labour Act, 1951
- Purpose: Addresses the health and safety of workers in plantations, including those involved in animal husbandry. (India code website)
- Key Provisions: Includes provisions for medical care and disease prevention among plantation workers, which indirectly affects zoonotic disease control.
10.The National Rural Health Mission (NRHM)
- Purpose: Focuses on improving healthcare delivery in rural areas, including services related to zoonotic diseases. (NHM website)
- Key Features: Includes vaccination programs, health education, and disease surveillance in rural settings.
- The National Livestock Mission (NLM)
- Purpose: Supports the development of the livestock sector, including measures to prevent livestock diseases. (NLM website)
- Key Features: Includes components for improving veterinary services, animal health infrastructure, and disease control.
12.The Hazard Analysis and Critical Control Points (HACCP) System
- Purpose: Though not specific to India, HACCP is implemented in various food safety standards that affect the handling of animal products. (FSSAI website)
- Key Features: Provides a systematic approach to food safety by identifying and controlling hazards in the food production process.
13.The National Policy on Biofuels
- Purpose: Addresses environmental and health impacts related to biofuels, including the use of animal and agricultural waste. (MNRE website)
- Key Features: Includes provisions for the safe handling and processing of biofuels to prevent contamination and zoonotic disease transmission.
14.The State Animal Husbandry Policies
- Purpose: Various states in India have their own policies on animal husbandry, which include measures for disease control and prevention.
- Key Features: State-specific guidelines for vaccination, disease surveillance, and biosecurity measures.
Implementation and Coordination:
- Central and State Governments: The implementation of these laws and policies involves both central and state governments. Coordination between various ministries (e.g., Ministry of Health and Family Welfare, Ministry of Agriculture and Farmers Welfare) is crucial.
- Agencies and Institutions: Bodies like the National Centre for Disease Control (NCDC), Indian Council of Agricultural Research (ICAR), and state veterinary departments play key roles in enforcement and monitoring.
These policies and laws, when effectively implemented and enforced, help in managing and preventing zoonotic diseases in India. Continuous updates and adaptations to these regulations are essential to address emerging zoonotic threats.
Prevention and Control Strategies
Effective prevention and control of zoonotic diseases require a multifaceted approach that integrates surveillance, early detection, rapid response, and public awareness. Key strategies include:
- Surveillance and Monitoring: Integrated surveillance systems combine human, animal, and environmental health data to monitor zoonotic diseases. These systems enhance early detection and response to outbreaks. Key components include data sharing, coordination between sectors, and the use of advanced technologies for real-time monitoring (Sapkota et al., 2007).
- Early Warning Systems- Early warning systems use data from surveillance programs to predict and detect potential outbreaks. These systems employ various tools, including statistical models, risk mapping, and remote sensing technologies, to provide early alerts and guide intervention strategies (Kausel et al., 2021).
- Cross-Sectoral Collaboration: Promoting collaboration between human health, animal health, and environmental sectors facilitates information sharing, resource allocation, and coordinated responses to zoonotic disease threats. Interdisciplinary research and partnerships strengthen capacity for disease surveillance, diagnostics, and outbreak response.
- Vaccination and Treatment: Vaccination of animals is a critical component of zoonotic disease prevention. Programs targeting diseases such as rabies, brucellosis, and leptospirosis help reduce the prevalence of these diseases and protect public health (Wortman et al., 2015). Examples of Successful Vaccination Programs include Rabies Vaccination: Widespread vaccination of domestic animals and wildlife to reduce the incidence of rabies and prevent transmission to humans; Brucellosis Vaccination: Immunization of livestock to control brucellosis and prevent its spread to humans; Leptospirosis Vaccination: Vaccination of livestock and pets to reduce the risk of leptospirosis transmission.Human vaccination programs target specific zoonotic diseases such as rabies, influenza, and other emerging infections. Vaccines play a crucial role in preventing disease outbreaks and reducing the burden of zoonotic infections (Hancock et al., 2009). Examples of Human Vaccination Programs include Rabies Post-Exposure Prophylaxis, Seasonal Influenza Vaccination, Ebola Vaccination.
- Education and Public Awareness: Raising awareness about zoonotic diseases, their transmission pathways, and preventive measures is crucial for fostering behaviour change and promoting community engagement. Educational campaigns should target healthcare workers, veterinarians, farmers, and the general public to encourage adoption of safe practices in agriculture, wildlife conservation, and food production.Public education campaigns aim to raise awareness about zoonotic diseases and promote preventive behaviours. Effective campaigns use various media platforms, including television, social media, and community outreach, to reach diverse audiences and encourage safe practices (Samaan et al., 2010). Community engagement involves working with local populations to promote zoonosis prevention. Strategies include community-based education programs, participatory approaches, and collaboration with local leaders to address specific health challenges (Cameron et al., 2015).
- Regulatory Measures: Implementing regulations and guidelines to mitigate high-risk practices in agriculture, wildlife trade, and food safety is essential for reducing the likelihood of zoonotic spillover events. This includes enforcing biosecurity measures, promoting sustainable farming practices, and regulating wildlife markets to minimize opportunities for pathogen transmission.
Challenges
Despite significant progress, several challenges hinder efforts to achieve the goals of One Health and effectively prevent zoonotic diseases. Limited resources and structure in numerous regions undermine the establishment and conservation of effective complaint surveillance and response systems. Addressing these gaps requires increased investment in public health structure, laboratory capacity, and healthcare pool training. The sustaining political commitment and fostering collaboration across sectors and authorities are essential for prostrating walls to effective complaint forestalment and control. Political leadership and transnational cooperation are critical for addressing global health pitfalls and promoting One Health principles on a global scale. Encouraging behavioural changes among stakeholders to borrow sustainable practices in husbandry, wildlife conservation, and food product is pivotal for reducing the threat of zoonotic complaint transmission. This requires targeted education, community engagement, and impulses to promote compliance with regulations and guidelines. Anticipating and responding to emerging infectious disease threats, including novel zoonotic pathogens with pandemic potential, requires proactive surveillance, rapid response capabilities, and adaptive management strategies. Investing in research and innovation is essential for developing new diagnostics, treatments, and vaccines to mitigate future health crises.
Future Directions
Looking ahead, integrating One Health principles into global health policies, enhancing research capacities, and fostering international cooperation are critical to mitigating the impact of zoonoses and safeguarding human, animal, and environmental health. By addressing the root causes of disease emergence and transmission, promoting sustainable practices, and investing in public health infrastructure, we can strengthen global health security and resilience against emerging infectious diseases. Collaborative efforts across sectors and disciplines are essential for achieving the goals of One Health and ensuring a safer, healthier future for generations to come.
Conclusion
“One World, One Health” embodies a vision of interconnectedness and collaboration in addressing global health challenges, particularly zoonotic diseases. By recognizing the shared vulnerabilities of humans, animals, and the environment, and by implementing proactive and integrated approaches grounded in the principles of One Health, we can build resilience against emerging health threats and promote sustainable health outcomes for all. As we navigate an increasingly interconnected world, the principles of One Health offer a pathway towards a healthier future for humanity and the planet.
References
- Bharti, A.R., Nally, J.E., Ricaldi, J.N., Matthias, M.A., Diaz, M.M., Lovett, M.A., Levett, P.N., Gilman, R.H., Willig, M.R., Gotuzzo, E. and Vinetz, J.M., 2003. Leptospirosis: a zoonotic disease of global importance. The Lancet infectious diseases, 3(12), pp.757-771.
- Cameron, A. R., et al. (2015). Community-Based Approaches to Disease Prevention. Global Health Action, 8(1), 28797.
- (2004). International Conference on Emerging Infectious Diseases (ICEID). Centers for Disease Control and Prevention.
- (2021). Salmonella Information. Centers for Disease Control and Prevention.
- Centres for Disease Control and Prevention (CDC). One Health Basics. Available at: [https://www.cdc.gov/onehealth/basics/index.html] (https://www.cdc.gov/onehealth/basics/index.html)
- Corbel, M.J., 2006. Brucellosis in humans and animals. World Health Organization.
- Department of animal husbandry and dairying, DAHD. Available at (https://dahd.nic.in/)
- Food and Agriculture Organization of the United Nations (FAO). One Health. Available at: [http://www.fao.org/one-health/en/] (http://www.fao.org/one-health/en/)
- Hancock, K., Veguilla, V., Lu, X., Zhong, W., Butler, E.N., Sun, H., Liu, F., Dong, L., DeVos, J.R., Gargiullo, P.M. and Brammer, T.L., 2009. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. New England journal of medicine, 361(20), pp.1945-1952.
- India Code. Available at (https://www.indiacode.nic.in/)
- Jackson, A.C., 2003. Rabies virus infection: an update. Journal of neurovirology, 9, pp.253-258.
- Jones, K. E., Patel, N. G., Levy, M. A., Storeygard, A., Balk, D., Gittleman, J. L. and Daszak, P. (2008). Global trends in emerging infectious diseases. Nature,451 (7181), 990-993.
- Kausel, E., et al. (2021). Technological Advances in Zoonotic Disease Surveillance. Journal of Epidemiology and Community Health, 75(6), 556-565.
- Mills, J.N., Ksiazek, T.G., Peters, C.J. and Childs, J.E., 1999. Long-term studies of hantavirus reservoir populations in the southwestern United States: a synthesis. Emerging infectious diseases, 5(1), p.135.
- Montoya, J. G., & Liesenfeld, O. (2004). Toxoplasmosis. The Lancet, 363(9425), 1965-1976.
- National animal disease reporting system, NADRS. Available at (https://nadrs.gov.in/)
- National health mission, NHM. Available at (https://nhm.gov.in/)
- National livestock mission, NLM. Available at (https://nlm.udyamimitra.in/)
- National rabies control programme, NRCP. Available at (https://www.rabiesfreeindia.mohfw.gov.in/)
- Peiris, J.S., Guan, Y. and Yuen, K., 2004. Severe acute respiratory syndrome. Nature medicine, 10(Suppl 12), pp. S88-S97.
- Perfect, J.R., Dismukes, W.E., Dromer, F., Goldman, D.L., Graybill, J.R., Hamill, R.J., Harrison, T.S., Larsen, R.A., Lortholary, O., Nguyen, M.H. and Pappas, P.G., 2010. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clinical infectious diseases, 50(3), pp.291-322.
- Samaan, M., et al. (2010). Public Health Campaigns. Journal of Public Health, 32(4), 567-574.
- Sapkota, A. R., et al. (2007). Integrated Surveillance Systems. International Journal of Environmental Research and Public Health, 4(2), 178-186.
- Taubenberger, J.K. and Morens, D.M., 2006. 1918 Influenza: the mother of all pandemics. Revista Biomedica, 17(1), pp.69-79.
- The Food Safety and Standards Authority of India, FSSAI. Available at (https://www.fssai.gov.in/)
- The Ministry of New and Renewable Energy, MNRE. Available at (https://mnre.gov.in/).
- United States Agency for International Development (USAID). PREDICT Project. Available at: [https://www.usaid.gov/news-information/fact-sheets/predict-project] (https://p2.predict.global/)
- (2016). Ebola Virus Disease Outbreak. World Health Organization.
- World Health Organization (WHO). One Health. Available at: [https://www.who.int/news-room/q-a-detail/one-health] (https://www.who.int/news-room/q-a-detail/one-health)
- World Organisation for Animal Health (OIE). One Health. Available at: [https://www.oie.int/en/for-the-media/onehealth/] (https://www.oie.int/en/for-the-media/onehealth/)
- Wormser, G.P., Brisson, D., Liveris, D., Hanincová, K., Sandigursky, S., Nowakowski, J., Nadelman, R.B., Ludin, S. and Schwartz, I., 2008. Borrelia burgdorferi genotype predicts the capacity for hematogenous dissemination during early Lyme disease. Journal of Infectious Diseases, 198(9), pp.1358-1364.
- Wortman, J. T., et al. (2015). Animal Vaccination Programs. Journal of Veterinary Medicine, 62(3), 148-154.