Understanding Acute Puerperal Metritis in dairy cattle and its therapeutic management
Nilendu Paul1*, Pradeep Nag BS1 1Phd. Scholar, ICAR-NDRI, Karnal
*Corresponding Author:
Nilendu Paul, Theriogenology Laboratory, SRS of ICAR- NDRI, Adugodi, Bengaluru.
Email: nilendu364@gmail.com
Introduction
Acute puerperal metritis (APM) is a systemic illness with pyrexia (rectal temperature >39.5°C) and signs of toxemia, usually occurs within 21 d after parturition and is characterized by an enlarged uterus and by an often foul-smelling, red-brown fluid to off-white purulent uterine discharge (Sheldon et al., 2006). It affects around 20% of lactating dairy cows, with the incidence ranging from 8% to more than 40% in some farms (Haimerl and Heuwieser, 2014).APM is one of the most detrimental post-partum diseases in dairy animals with severe consequences in future reproductive performances and incurs huge loss to the dairy farmers/ farm. LeBlanc et al. (2002, 2008) reported that APM compromises future reproductive performances by increasing generation interval, increased milk discard and increased culling.Escherichia coli, Trueperella pyogenes, Fusobacterium necrophorum, and Prevotellamelaninogenica are thought to be primary pathogens causing uterine disease, because these bacteria were frequently isolated from the uterine lumen of APM affected cows. As APM mostly occurred due to bacterial infections, antibiotics are recommended for treating the condition. Antibiotics generally used for treating puerperal metritis include penicillin, 3rdgeneration cephalosporins, or a combination of ampicillin with oxytetracycline or cloxacillin (Naket al., 2011). Choosing a suitable antibiotic alone or in a combination is crucial as there is every chance of developing antibiotic resistance implying to the emergence of resistant bacteria.
Etiology
1. Bacteroides: B. heparinolyticus
2. Porphyromonas: Porphyromonaslevii, Porphyromonasendodontalis, andPorphyromonassomerae
3. Fusobacterium: Fusobacterium necrophorum
4. Escherichia coli
5. Trueperella pyogenes
6. Helcococcus: HelcococcusovisandHelcococcuskunzii
Uterine microbiota structure remains nearly identical between cows that developed metritis and healthy cows until 2 days post-partum(DPP), then bacterial structure deviates favoring greater relative abundance of Bacteroides, Porphyromonas, and Fusobacterium in metritic cows.
Clinical signs and symptoms
Affected cows are depressed, febrile, a systemic illness with fever (rectal temperature >39.5°C) and inappetence. A fetid, red-brown and watery uterine discharge is characteristic of the condition in cows but may not be conspicuous in other species. Milk production is reduced and nursing young calf may show signs of food deprivation.
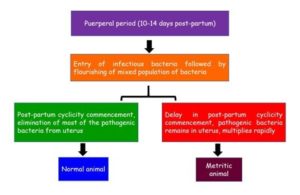
Pathogenesis
No single gold standard is available to identify metritis; thus, a combination of signs is used to diagnose this postpartum disease. Following signs are helpful in diagnosing the case
Systemic signs of health disorders: poor appetite, low production, and dull attitude.
Fever: rectal temperature above 103°F.
Abnormal vaginal discharge: watery, foul-smelling, and brownish.
Inserting gloved hand inside vagina of the cow and vaginal contents are slowly collected and evaluated.
Using the Metricheck device (Fig-1)to diagnose metritis. Previously mentioned gloved hand method is similar to the procedure of the Metricheck.

The Metricheck device provides a very economically effective way to evaluate vaginal discharge in field condition. The device consists of a stainless-steel rod with a rubber hemisphere to retrieve the vaginal contents. The Metricheck device is cleaned with a non- irritant and non-corrosive disinfectant, inserted into the vagina of the cow, and then gently removed by pulling the device backward at an upward 45° angle.
After the vaginal content is collected, scoring is done based on its quality and smell of the mucus (Fig-2)
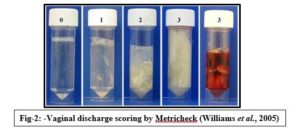
Using this scoring system, the mucus can be described as:
Score 0 = clear or translucent mucus;
Score 1 = mucus containing flecks of white or off-white pus;
Score 2 = discharge containing ≤50% white or off-white mucopurulent material;
Score 3 = discharge containing ≥50% purulent material, usually white or sanguineous.
Treatment
1.Most commonly used treatment strategies for metritis use either intrauterine antibiotics or systemic antibiotics or both. Systemic antibiotics are more widely approved and effective in dairy cows than intrauterine antibiotics. Intrauterine antibiotics loses its potency in contact with purulent material, also it competes with the innate uterine immune response to eliminate intrauterine pathogens thus intrauterine therapy is not indicated till 30 days after parturition. Promising systemic antibiotics are third-generation cephalosporins i.e. ceftiofur hydrochloride, ceftiofur sodium, and ceftiofur crystalline free acid. Out of these, crystalline free acid tends to be the favorite choice because of itslong-lasting effects. Treatment for metritis is advocated when the cow has a combined Metricheck score and smell score above 3.
2.APM responds well to systemic antimicrobial therapy when combined with NSAIDs and supportive fluid therapy. Third-generation cephalosporin antibiotics or penicillin are considered most suitable for systemic treatment of cows with metritis because of their activity against most common pathogens, reaches therapeutic levels in endometrial tissues, maintains optimum drug concentration in endometrium tissue and may help preventing potential sequelae of metritis and endometritis, such as endocarditis or renal disease.
3.Oxytetracycline requires administration at high dose (11 mg/kg, bid) for maintaining uterine tissue concentrations of 5 mcg/g, which is below the minimal inhibitory concentration (MIC) for many strains of pathogenic T pyogenes.
4.Drainage of the uterine content may be advantageous but should be advocated only after initiation of antimicrobial therapy and should be done very gently because the inflamed uterus may be friable, more prone to rupture and manipulation of the uterus may result in bacteremia.
Conclusions
Acute puerperal metritis (APM) is a systemic illness in dairy cows, usually occurs within 21 days post-partum with systemic signs such as febrile condition, pyrexia, toxaemia with fetid red-brown discharge from vagina. APM is detrimental to the future reproductive performance of the affected animals and dairy farmers bears a huge economic loss in terms of reduced milk yield and increased calving interval. Diagnosis is based onsystem signs of illness and visualizing the purulent discharge from vagina and scoring them. Recent treatment strategies primarily focus on eliminating the uterine pathogens without hampering the innate uterine immunity. Therefore, treatment consists of systemic administration of third-generation cephalosporins or penicillin group antibiotics, that are of great value as compared to intrauterine therapy. As the period after parturition is crucial for both dam as well as to the new born calf, dairy farmers are advised to maintain the calving area clean and hygienic that will definitely reduce the occurrence of uterine diseases.
Author’s declaration
The authors declare that this article has not been previously published anywhere.
References
1. Haimerl, P., &Heuwieser, W. (2014). Invited review: Antibiotic treatment of metritis in dairy cows: a systematic approach. Journal of dairy science, 97(11), 6649-6661.
2. LeBlanc, S. J., Duffield, T. F., Leslie, K. E., Bateman, K. G., Keefe, G. P., Walton, J. S., & Johnson, W. H. (2002). The effect of treatment of clinical endometritis on reproductive performance in dairy cows. Journal of Dairy Science, 85(9), 2237-2249.
3. LeBlanc, S. J. (2008). Postpartum uterine disease and dairy herd reproductive performance: a review. The Veterinary Journal, 176(1), 102-114.


