BLOOD TRANSFUSION IN CATTLE
Dr Amit Bhardwaj,Vet Surgery specialist,Pune
Introduction
Blood transfusion is being practiced for centuries for saving life
of human beings and animals. Richard Lower in 1665 transfused
the blood in a dog for the first time in the history . With the
help of latest techniques and equipment developed after 1950,
blood transfusion became more popular in veterinary medicine
. Blood transfusion has made considerable advancements in
veterinary medicine in recent times. Although, the information and
availability of blood and its products has increased, transfusion
therapy has become more complex. Advanced screening facilities,
blood group testing and techniques for cross matching blood
had made the process of donor selection more complicated.
Advancement in techniques of separating the components of
blood has given the clinician an opportunity to use the component
as per the demand of the patient. This article summarizes recent
advances in veterinary transfusion medicine and guides the
clinicians in decision making while transfusion with evidence
The need for blood transfusions is acute, as in acute hemolysis or hemorrhage; transfusions are also appropriate in treatment of acute or chronic anemias. Animals with hemostatic disorders often require repeated transfusions of whole blood, red cells, plasma, or platelets. Blood transfusions must be given with care, because they have the potential to further compromise the recipient.
Whole blood frequently is not the ideal product to be administered. If the need is to replace the oxygen-carrying capability of the blood, then packed RBCs are more appropriate; if replacement of circulatory volume is needed, crystalloid or colloid solutions may be used, with packed RBCs added as needed. Platelet numbers rise rapidly after hemorrhage, so replacement is rarely needed. Plasma proteins equilibrate from the interstitial space, so plasma is not needed except in massive hemorrhage (>1 blood volume in 24 hr). Animals that require coagulation factors benefit most from administration of fresh-frozen plasma or cryoprecipitate if the need is specifically for factor VIII, von Willebrand factor, or fibrinogen. Platelet-rich plasma or platelet concentrates may be of value in thrombocytopenia, although immune-mediated thrombocytopenia usually does not respond to administration of platelets because they are removed rapidly by the spleen.
The decision to transfuse RBCs is determined by clinical signs, not by any pre-selected PCV. Animals with acute anemia show signs of weakness, tachycardia, and tachypnea at a higher PCV than animals with chronic anemia. The amount of RBCs required to relieve clinical signs will generally increase the PCV above 20%. Domestic animals have blood volumes of 7%–9% of their body weight; cats have a slightly lower volume of ~6.5%. By determining the recipient’s blood volume and knowing the animal’s PCV, the required replacement RBC volume can be calculated. For example, a 25-kg dog has a total blood volume of ~2,000 mL; with a PCV of 15%, the RBC volume is 300 mL; if the PCV is to be increased to 20%, that equals an RBC volume of 400 mL. Therefore, 100 mL of RBCs or 200 mL of whole blood (with PCV of 50%) would be required to increase the recipient’s PCV to the desired level. These calculations assume no ongoing losses of RBCs through hemorrhage or hemolysis. Obviously, the post-transfusion PCV is the most important measure of adequacy of red cell dose. No more than 20% of a donor animal’s blood should be collected at one time.
Collection, storage, and transfusion of blood must be done aseptically. The anticoagulant of choice is citrate phosphate dextrose adenine (CPDA-1). Commercial blood bags containing the appropriate amount of anticoagulant for a “unit” (500 mL) are available. Heparin should not be used as an anticoagulant, because it has a longer half-life in the recipient and causes platelet activation; also, heparinized blood cannot be stored.
Blood collected in CPDA-1 with added RBC preservation or nutrient solutions may be safely stored at 4°C for 4 wk. If the blood will not be used immediately, the plasma can be removed and stored frozen for later use as a source of coagulation factors or albumin for acute reversible hypoalbuminemia. Plasma must be frozen at –20° to –30°C within 6 hr of collection to assure that levels of factor VIII are adequate and will remain so for 1 yr. Chronic hypoproteinemia is not helped by plasma, because the total body deficit of albumin is so large that it could not be improved by the small amount contained in plasma. Colloid solutions such as hetastarch are more effective for treatment of hypoalbuminemia. Human albumin has been used in dogs; however, the risk of sensitization and allergic reactions is significant.
Purpose
• Live-saving therapy in cases of life-threathening anaemia in cattle
• Relatively simple to perform
• Procedure takes 60 to 80 minutes
• Spectacular results
• Low cost possible
• Economically justifiable
Facts and figures
• Normal blood volume: 8 % of BW
• Normal adult bovine PCV: 24 – 43 %
• Haemorrhagic shock when 30 – 40 %
of the total blood volume is lost rapidly
• A cow with a PCV of 10 % will have lost two-thirds of
its circulating red cells
• One litre blood will raise up the PCV with +/- 0,75 %
• The clinical difference between a cow with a PVC
of 8 % and a cow with 14 % is remarkable
• Turn over of red cells is not very long(2 à 3 days)
• Repeated transfusions can cause reactions, red cell
survival only a few hours
Indications
• Acute haemorrhage
– Rupture of a.vaginalis after(severe) extraction
– Complication after caesarian sectio
– Uterusprolaps
– Umbilical vesseldamage by a newborn calf
– Trauma
• Abomasal ulceration
– Anaemia and melena
• Redwater:
– Tickborn protozoan parasite (Babesia divergens)
– Destruction of erythrocytes
Procedure
• Donor cow:
– Quiet to handle
– Healthy
– Not heavily pregnant
– Large animal with a normal BCS
– Non-lactating, since the administration of xylazine
will necessitate a milk withholding period
Equipment required
– Xylazine -Procaine -Scalpel
– Large bore needle-Tourniquet – Funnel
– Na-citrate – Physiological serum
– Collapsible plastic containers for blood collection
Blood collection
• Restraint is achieved using a halter,
• Head tied up
• Sedation: xylazine
• Prepare the collection site in the mid-jugular
area
• Local anaesthesia
• Small incision in the skin
• Some anaesthetic subcutaneously around jugular vein
Collection
• Large bore needle (diameter 4 – 5 mm)
• Raise the vein with tourniquet( chain, rope with small round block or digital pressure)
• Insert the large bore needle trough the skin incision and into the jugular vein
• Blood collected by using a funnel inserted into the top of the collection vessel (plastic
waterbottles 1.1/2 ltrs) with anticoagulans
• Agitate gently the collected blood to mix it with the anticoagulanssolution
• Look out for contamination
• After collection of 5 to 8 litres(+/- 10 min), release pressure and remove needle
• Close the skin with a couple sutures
• For small amounts(450 ml), use human disposable vacuumbags(Terumo)
Anticoagulants solution
• Sodium citrate:
– 100 ml of a 3.8 to 5 % per litre blood
– Make it freshly up : physiological serum with the sodium
citrate (crystalline powder)
• Heparin sodium:
– Solution 5000 units in 5 ml vials
– 5000 units for 1 litre blood
• Before collecting :coat the needle and funnel with the anticoagulanssolution, otherwise bloodclothforming during collection possible
• Collected blood should be used within two hours
Administration of blood
• Restraint the recipient animal
• Sedation mostly not necessary
• Prepare the insertion area
• Local anesthesia
• Small skin incision
• Insert a 12 gauge 8 cm catheter and suture in place
• Attach the giving set to the catheter
• Transfusion of 5 to 8 litres will take 30 to 45 minutes
• Monitor transfusion reactions
• Blood may be given intraperitoneally, red cells will taken up in
an unaltered state, absorption is relatively slow
Transfusion reactions
• Bovine blood 13 major types
• Bovine red cells don’t agglutinate easily
• Most important factors: haemolysins
• Preformed isohaemolysins not present or in a very low quantity
• Repeated transfusions within seven days more risk for reaction
Transfusion reaction signs
Usually reactions are rare and mild
• Increase of respiratory rate
• Hiccuping
• Sweating
• Tachycardia
• Violent movements
• Severe respiratory distress
• Coma and death
• Treatment: adrenaline 5 ml (1: 1000, 1mg/ml solution) IM or cortico’s
Major Blood Groups of Clinical Interest
Species Blood Group
Canine DEA 1.1 and 7
Feline A, B, mic
Equine A, C, Q
Blood groups
Blood groups are named according to the species-specific
antigens present on the surface of erythrocytes. Theses
antigens play an important role in inducing immune-mediated
reactions and can cause complications while transfusing blood
from different blood groups. Antigens coupled with platelets,
leukocytes and plasma proteins may also induce immune
mediated reactions in host animals during transfusion therapies
Plasma also has some naturally occurring all antibodies that can
act against other blood groups without any prior exposure to the
erythrocyte antigens. Erythrocyte antigens can induce production
of antibodies when animals get exposed via blood transfusion,
transplacental exposure or in the case of neonatal isoerythrolysis
(NI), through colostrum. Blood groups in the common domestic and pet animal species are described here. From a clinician’s point of view, these are the antigens to which the veterinary practitioner should be most familiar. However, many other blood group factors and systems have been described and the lack of commercially available typing sera does not diminish the potential significance of these other systems in transfusion medicine.
Cattle:
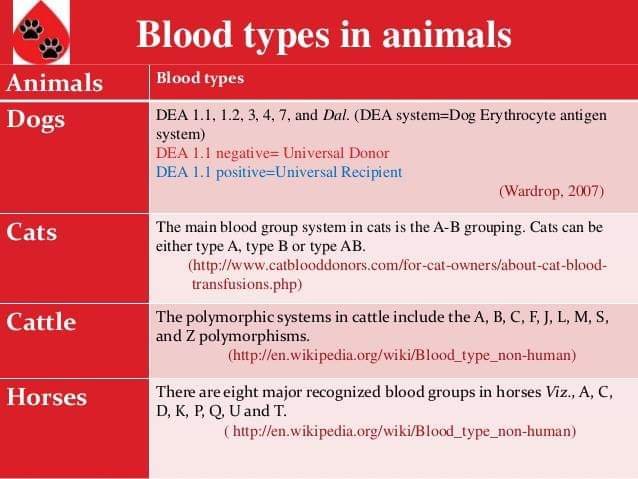 The internationally recognized blood groups in cattle are A, B,
The internationally recognized blood groups in cattle are A, B,
C, F, J, L, M, R, S, T and Z. out of these 11 groups, group B and J being
the most clinically relevant. The B group itself has more than 60
antigens, thereby making closely matched blood transfusions
difficult. The J antigen is not a true erythrocyte antigen but a
lipid found in plasma Cattle having anti-J antibodies with a small
amount of adsorbed J antigen on erythrocytes but negative J
blood group, can develop transfusion reactions when receiving.
Reference:On request


