Dog Cancer :Chemotherapy Treatment Procedure in Dogs
Chemotherapy, often referred to as “Chemo”, is a treatment procedure that uses chemicals or drugs to kill cells in humans, dogs, and other animals. The cells are either microorganisms (such as bacterial) or cancer cells. By definition, chemotherapy can refer to either antibiotics or anti-cancer drugs.
The most common use of the word “chemotherapy” is as a drug or drugs used to treat cancer. Chemotherapy can refer to the use of one drug or a combination of drugs. The specific drugs or drugs used depends on the type of cancer and what drugs are most effective to battle that type of cancer.
Each type of cancer is studied to determine the most effective treatment combination. Based on this research and the specific type of cancer, chemotherapy recommendations for your dog’s particular situation will be given by your veterinarian.
Chemotherapy can be used alone, before or after surgery, or with or without radiation therapy.
The goal of chemotherapy is to kill tumor cells that stop or kill tumor growth and therefore either minimizing or eliminating the cancer and therefore giving your dog an extended life.
Another goal is to give a chemotherapy dose that will minimize side effects therefore allowing your dog to maintain a good quality of life while maximizing the drugs effect on the cancer cells.
Chemotherapy is a term given to a group of drugs that have the ability to kill cancer cells in dogs. The specific medication or combination will depend on the type of cancer your dog has, as well as his overall health. Your vet will monitor the chemotherapy treatment to ensure that it is working well with minimal side effects. If not, he or she might try another drug or change the dosage and frequency.
Cancer is often unpredictable, and as a result, may require a variety of treatment modalities. As with people, surgery, radiation therapy, and chemotherapy are commonly used alone or in combination with other treatments to control cancer in pets. Chemotherapy may be used to treat cancer that has spread to other parts of the body, to treat cancer that cannot be treated with surgery or radiation therapy alone, or when it may enhance the effectiveness of these treatments. Chemotherapy treatment for pets with cancer is supervised by a medical oncologist, a veterinarian with five years of specialty oncology training. Flint Animal Cancer Center’s medical oncologists are board-certified and specially trained to diagnose cancer in pets and prescribe treatment while monitoring for side effects and making the appropriate adjustments to ensure each pet patient maintains a good quality of life.
The prospect of chemotherapy for your pet may be intimidating or even scary. The good news is that pets typically handle chemotherapy much better than people. Knowing how chemotherapy drugs work and what to expect from the treatments can help you decide whether this therapy is right for your pet. The following represent some of the most common questions relating to chemotherapy for pets with cancer.
Chemotherapy is often prescribed for one of the most common cancers in dogs, lymphoma, as well as for some other malignancies.Chemotherapy is recommended for cancers that either have already spread to other areas of the body (metastasized) or are known to have a high potential for metastasis. The goal of chemotherapy in animals is different than for humans, which is why treatment is less aggressive. With pets, the primary goal of chemotherapy is to provide your cat or dog with the best quality of life for as long as possible. With the goal of clearing up cancer or preventing it from spreading, chemotherapy treatment works by attacking growing cells. The cells are targeted whether they’re cancerous or not. Chemo is meant to either kill the cells or stop them from dividing.
Chemotherapy may be offered alone or along with other interventions, such as surgery or radiation. Drugs may also be given orally as a pill your dog can swallow. Chemo may be administered via an injection at a veterinary appointment.
Chemotherapy is drug therapy designed to kill or slow the growth of cancers. Many of the drugs used to treat cancer are derived from natural substances such as plants, trees or even bacteria and are often the same drugs used in people. Some drugs have a broad spectrum of activity, while others are more targeted.
Chemotherapy may be used as the primary treatment for certain cancer types, or may be used in combination with other treatments such as surgery and radiation therapy. In some cases, chemotherapy can be used to try to shrink large tumors prior to surgery, or to help eliminate microscopic cancer cells that cannot or have not been completely removed surgically. For cancers that are at high risk for spread, chemotherapy can be used after surgery to help delay or prevent the appearance of cancer in other parts of the body.
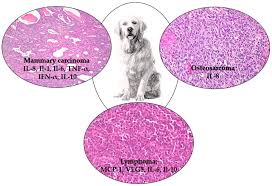
Common Types Of Cancer In Dogs
Unlike many other species of animals, dogs are susceptible to the same types of cancer as humans. Cancer is caused by the uncontrolled growth of cells in the body. These cells can originate in any of the body’s tissues. If not found and arrested in time, cancer can expand and connect with the circulatory or lymph systems, and also can spread and infect other tissues in the body. Canine cancer is the leading cause of death for dogs 10 years of age and older. However, half of all cancer in dogs is treatable if it is arrested in its early stages.
The most common types of cancer in dogs are:
- Hemangiosarcoma:This form of dog cancer is an incurable tumor of cells that line blood vessels, called endothelial cells. Although dogs of any age and breed are susceptible to Hemangiosarcoma, it occurs more commonly in middle aged or elderly dogs. Also certain breeds have a much higher incidence including Golden Retrievers and German Shepherds. For this reason, we may recommend additional screening for these breeds after age 7. This form of dog cancer develops slowly and is essentially painless, so clinical signs are usually not evident until the advanced stages when the tumors are resistant to most treatments. Less than 50% of treated dogs survive more than six months, and many die from severe internal bleeding before there is an opportunity to institute treatment.
- Mast Cell Tumors:These are immune cells that are responsible for allergies. Mast cells can be found in all tissues of the body but typically form tumors on the skin in close to 20 percent in the canine population. They range from relatively benign to extremely aggressive. Certain breeds of dog are at an increased risk for the development of this tumor, indicating that genetics might be a cause. Boxers are especially prone to this type of cancer.
- Lymphoma:This form of dog cancer can affect any dog of any breed at any age. Most of the time, it appears as swollen glands (lymph nodes) that can be seen or felt under the neck, in front of the shoulders, or behind the knee. Occasionally, lymphoma can affect lymph nodes that are not visible from outside the body, such as those inside the chest or in the abdomen. This can cause trouble breathing and digestive trouble. Generally this form of dog cancer is considered treatable if arrested in its early stages. Standard Poodles, Golden Retrievers and Australian Shepherds are a few of the breeds with higher incidence of lymphoma.
- Osteosarcoma:This form of dog cancer is the most common type of primary bone cancer in dogs, accounting for up to 85% of tumors that originate in the skeletal system. Although it mostly affects older large or giant breed dogs, it can affect dogs of any size or age. Osteosarcoma occurs in many areas, but it most commonly affects the bones bordering the shoulder, wrist and knee. A major symptom is lameness in the affected leg, or a swelling over the area that seems painful at the site.
- Brain Tumors:Epileptic-like seizures or other extreme behavioral changes are usually the only clinical signs of a brain tumor. CAT scanning and MRI at a veterinary specialist is used to determine location, size and severity. Although some oral chemotherapy and radiation therapy can control some inoperable tumors, surgical intervention may be recommended if the tumor is operable.
- Bladder Cancer:Some breeds are more at risk for this form of dog cancer than others. This is a slow developing dog cancer, and symptoms may not show for 3 to 6 months. Urinary obstruction and bleeding are common symptoms.
- Mammary Carcinoma:Non-spayed female dogs are at high risk for developing malignant mammary tumors, but all female dogs regardless of reproductive state remain at risk. Approximately 50% of these tumors are malignant, and complete surgical removal is recommended if the cancer has not metastasized.
- Malignant Histiocytosis:This dog cancer affects larger sport breeds most often. It occurs as localized lesions in the spleen, lymph nodes, lung, bone marrow, skin and subcutis, brain, and periarticular tissue of large appendicular (limb) joints. Histiocytic sarcomas can also occur as multiple lesions in single organs (especially spleen), and rapidly disseminate to involve multiple organs. Unfortunately there is no reported effective therapy for this form of dog cancer.
- Squamous Cell Carcinomas:It is most often found in the mouth and the nail beds of the toes. Early detection and complete surgical removal is the most common treatment. Fewer than 20% of dogs develop metastatic disease. SCC of the tonsil and tongue are quite aggressive and fewer than 10% of dogs survive 1 year or longer despite treatment measures.
- Mouth and Nose Cancer:This is a very common form of dog cancer, more so in the mouth than the nose. Symptoms include a mass on the gums, bleeding, odor, or difficulty eating. Since many swellings are malignant, early, aggressive treatment is essential. Cancer may also develop inside the nose of dogs. Bleeding from the nose, breathing difficulty, or facial swelling are symptoms that may indicate nose cancer.
- Melanoma:This form of dog cancer most commonly occurs in canines with dark skin. Melanomas arise from pigment producing cells called melanocytes, which are responsible for coloring the skin. Melanomas can occur in areas of haired skin, where they usually form small, dark (brown to black) lumps, but can also appear as large, flat, wrinkled masses. Malignant melanoma, which develops in the mouth or in the distal limbs (usually the toenail beds), is an incurable disease. These tumors have very often spread to distant parts of the body by the time they are first noticed, making complete surgical removal impossible.
- Testicular:This form of dog cancer is common in unneutered dogs or in dogs with retained testes. This form of dog cancer is largely preventable with neutering, and curable with surgery if arrested early in the disease process.
Symptoms And Signs Of Cancer In Dogs
Some signs of cancer in dogs are easy to spot and others are not. Signs of cancer in dogs may vary greatly depending upon a number of factors. However, the following list identifies some of the most common signs of cancer in dogs:
- Lumps and bumps underneath a dog’s skin
- Abnormal odors emanating from the mouth, ears or any other part of the body
- Abnormal discharge from the eyes, mouth, ears or rectum
- Abdominal swelling
- Non-healing wounds or sores
- Sudden and irreversible weight loss
- Change in appetite
- Coughing or difficulty breathing
- Lethargy or depression
- Changes in bathroom habits
- Evidence of pain
What You Need To Know About Tumors In Dogs
Tumors in dogs usually appear as fleshy but solid lumps of tissue underneath a dog’s skin and fur. Not all tumors will be outwardly evident. Sometimes you can see evidence of tumors and sometimes they are deep within the body of the dog. However, early detection and treatment are key to preserving your dog’s health and quality of life. Therefore, it is important to periodically inspect your canine companion for any abnormal lumps and keep a semi-annual veterinary appointment schedule.
Owners most commonly find a tumor on their dog while petting or bathing. If you are running your hand over any part of your dog’s body and feel a lump, call to make an appointment with your veterinarian. Most likely, the veterinarian will want to do a needle aspirate to get cells from the tumor to get a diagnosis on the type of tumor. The diagnosis is helpful in determining what if any type of surgery and or follow up cancer care may be necessary. Some tumors in dogs cannot be visualized but can be palpated (felt with touch) by your veterinarian during the exam. For instance, an enlarged spleen may be palpable to your veterinarian but not visible to the owner. You can reference the list of canine cancer symptoms above to get a better understanding of what symptoms to be on the lookout for.
Diagnosing Canine Cancer
Only a veterinarian can accurately diagnose canine cancer. This is why it is extremely important to schedule periodic wellness exams for your canine companion. During these preventive exams, your veterinarian can check your dog for signs of canine cancer. Treating canine cancer before it advances is key to successful recovery.
Treatment Options For Dogs With Cancer
Several factors influence cancer treatment decisions for dogs with cancer, including:
- Age of the dog
- General health of the dog
- Tumor type
- Biological behavior of the tumor
- The Stage of the Cancer
The patient’s overall health status plays a major role in therapy choices for dogs with cancer. This includes evaluating the patient for his or her ability to tolerate cancer treatment. Life expectancy should be taken into consideration as well; for a slow-growing tumor in an older dog, for example, treatment drawbacks may outweigh potential benefits.
Treatments for dogs with cancer are similar to human therapies, which can include:
- Chemotherapy
- Surgery
- Radiation therapy
- Holistic or herbal therapy
There is a lack of consensus as to whether you must choose only one course of treatment, or if multiple treatment options can be combined effectively. Sometimes combining methods works well for dogs with cancer, but that may not always be the case as some treatments may interfere with each other and potentially cause unintended harm. These are important issues to address with the veterinarian at your next appointment.
Chemotherapy Procedure in Dogs
Some chemotherapy is simply given in the form of a pill which your dog will ingest. This can either be given at home or by your veterinarian. For other forms of chemotherapy that are intravenously administered, your pet will need to visit your veterinarian. Your veterinarian will place a small catheter into your pet’s vein through which the chemotherapeutic agent will be delivered. Some chemotherapy agents need to be delivered slowly while others can be administered more rapidly. You can expect your dog’s chemotherapy session to last between 30 minutes and 2 hours. Depending on the type of cancer and chemotherapy protocol, your dog may need to return for more chemotherapy. Chemotherapy protocols range in span from a few weeks to several months.
Efficacy of Chemotherapy in Dogs
The efficacy of chemotherapy is dependent on the type of chemotherapy and the goals of the owner and veterinarian and oncologist. Chemotherapy is most effective when a combination of different agents and, if warranted, surgery are used together. The effects of chemotherapy are permanent on those cancer cells that it has damaged. In some cases, the dog has an aggressive or advanced cancer and the goal of chemotherapy is not for remission but palliative. Treatments related to chemotherapy include surgical resection and radiation therapy. Surgical resection alone serves to debulk any large tumors, however, microscopic disease may remain behind. Radiation therapy targets cancer cells but is not effective alone for large tumors in dogs. The most effective cancer treatment often involves a combination of several techniques as they all have their strengths and weaknesses.
Chemotherapy Recovery in Dogs
Chemotherapy is a non-invasive procedure so your dog will be in and out of the veterinarian’s office the same day. Recovery from chemotherapy involves the management of side effects of the chemotherapeutic agents. Most commonly seen side effects are nausea, vomiting, and diarrhea. Your veterinarian will give your dog anti-nausea medication if they exhibit these side effects. Chemotherapy can also lower your dog’s white blood cell count so your dog will have white blood cell counts taken at subsequent chemotherapy visits. Some chemotherapeutic agents can affect your dog’s liver or kidneys. If one of those agents is being used, your veterinarian will order liver or kidney blood work to ensure that they remain healthy during the course of chemotherapy.
HOW IS CHEMOTHERAPY GIVEN?
There are different formulations of chemotherapy. Some drugs must be given intravenously (IV), others may be given under the skin or into a muscle. In some cases the drug may be injected directly into the tumor itself. Some chemotherapy can be given orally in pill form.
IV drugs: Such as vincristine or doxorubicin; an intravenous catheter must be placed for safe administration of the drug. After administration, the catheter is removed and a light bandage is placed. The “band-aid” can be removed 1-2 hours after the drug is administered.
Oral drugs: Oral drugs are administered by you at home. It is important that your pet receive all medications as prescribed and that the pills are not crushed or split, nor capsule opened. It is sometimes helpful to coat the pills with butter, peanut butter or cream cheese to make it more appealing for your pet. If you are administering an oral chemotherapeutic drug, you will be given latex gloves to wear while you handle these pills. When you are finished giving the pills, wash your hands to remove any medication residue from your skin.
WHAT SORT OF SIDE EFFECTS MAY MY PET HAVE WITH CHEMOTHERAPY?
The highest quality of life for your pet is our goal, but to be effective in controlling a devastating disease like cancer, chemotherapy drugs are very powerful. Fortunately, pets don’t have as many side effects as humans going through chemotherapy do. In fact, 70% of pet patients face few, if any side effects. Hair loss (alopecia), is common in humans but rare in dogs. It is seen mainly with breeds that have constantly growing hair (poodle, shih tzu, cocker spaniel, etc.). Cats generally do not lose body hair, but often lose their whiskers. Chemotherapy will slow the re-growth of hair in all pets receiving chemotherapy so grooming schedules may need to be adjusted accordingly. Other potential side effects include nausea, vomiting, diarrhea – most of which are readily controlled with medications / diet change and only last for a day or two. A common side effect with many chemotherapy treatments is a decrease in the white blood cell count. This could make your pet more susceptible to contracting infections if the decrease is severe.
HOW SHOULD I HANDLE BODY FLUIDS WHILE MY PET IS ON CHEMOTHERAPY?
Do not handle feces, urine or vomitus unless absolutely necessary within 24 hours of the chemo administration. If your pet has an “accident”, wear gloves and clean the area with disposable items (paper towels, baby diapers, etc.) and dispose in the trash. Wash your hands thoroughly when you are finished cleaning. In general, it is recommended that clothing/ bedding which is soiled by feces, urine or vomitus within 24 hours of chemotherapy administration should be washed twice in hot water.
HOW OFTEN IS CHEMOTHERAPY GIVEN?
Some drugs are given daily, others weekly and some only every 2-3 weeks. Your time commitment will depend on the chemotherapy drug protocol you choose to treat your pet with.
WHAT IS A CHEMOTHERAPY DRUG PROTOCOL?
The word protocol refers to a set regime of drug(s) given in a specific time frame. This may incorporate one or multiple drugs.
HOW LONG WILL MY PET RECEIVE CHEMOTHERAPY?
Many chemotherapy protocols involve a series of treatments, followed by a period of careful observation. However, in some patients with advanced disease, chemotherapy may be continued as long as it is controlling the cancer.
WHAT HAPPENS WHEN CHEMOTHERAPY NO LONGER CONTROLS THE CANCER?
Cancers can be initially very sensitive to chemotherapy drugs. Unfortunately, the cancer may return weeks, months or years later. In such cases, the cancer cells have become resistant to the drugs in a similar way bacteria become resistant to antibiotics. When resistance to one drug occurs, we can often use other drugs. However, each time resistance develops it becomes more difficult to find a drug that the cancer will respond to. In some cases, cancer develops resistance to all drugs. At this point, your pet’s clinician will discuss with you ways to keep your pet comfortable for the remainder of his/her life.
Side Effects
Almost all chemotherapy agents have the potential to induce side effects, but they would not be used if their potential benefits did not outweigh the possible risks. Unlike people receiving chemotherapy, the vast majority (80-90%) of dogs and cats have minimal to no side effects. However, a small number of patients may have moderate to severe side effects. Rarely is a side effect life-threatening to the patient.
Chemotherapy side effects occur as a result of the toxic effects that chemotherapy agents have on the normal cells in the body. The majority of the normal cells that may be affected are found in the lining of the intestines (GI tract) and in the bone marrow. There may be other specific toxicities associated with various chemotherapy agents on particular organs, and these will be discussed when indicated.
The common side effects associated with the GI tract include vomiting, diarrhea and nausea/loss of appetite. The common side effects associated with the bone marrow include a decrease in the white cell count leading to immunosuppression (a compromised ability of the body to fight infection), loss of appetite and lethargy. It is rare to affect other bone marrow-derived cells such as the platelets and red blood cells.
Many side effects, such as those associated with the GI tract, are not immediate and become evident three to five days after chemotherapy. In the majority of cases, the side effects are limited to no more than 24 to 48 hours. The white cell count is typically at its lowest point 7 to 10 days after treatment, and the cells naturally rebound quickly. If needed, medications can be administered to counteract these side effects.
What Potential Side Effects May Come from My Pet Receiving Chemotherapy?
Potential side effects of chemotherapy occur as a result of normal cells being killed by the chemotherapy agents. The side effects are associated with organs that have the fastest turn-over (ie rapidly dividing cells), which in the normal body are the bone marrow and the gastrointestinal tract. Other side effects are possible depending on the specific drug and usually involve an additional organ. Although serious side effects can occur with any chemotherapy, there is a low risk for hospitalization for side effects (10% chance), and less than a 1% chance of life-threatening side effects. Here are examples of commonly encountered side effects from chemotherapy:
- Reduced White Blood Cell Count: Many chemotherapeutic agents affect the bone marrow, and the white blood cell that is most rapidly affected is the neutrophil. As discussed above, the neutrophil is the white blood cell that helps fight infection, and a decrease in the number of circulating neutrophils is called neutropenia. Neutropenia usually occurs 7-10 days after most chemotherapy administration. Should the neutrophil count be too low for chemotherapy, the doctor may wish to perform periodic blood tests (Complete Blood Counts), delay a scheduled therapy, prescribe prophylactic antibiotics to protect against infection or recommend hospitalization for those animals that are sick.
- Gastrointestinal Discomfort: Patients experience some form of GI discomfort typically 2-7 days after chemotherapy. These signs tend to be self-limiting and mild. Many times, changing to a bland diet, offering smaller meals throughout the day and the use of medications to help with the signs of discomfort is sufficient. We typically prescribe medications to address anticipated gastrointestinal signs in advance of therapy, or we will supplement with these medications if side effects have been encountered:
- Nausea: Signs of nausea include: lip-smacking, drooling, eating grass (unless this is normal for your pet), or loss of appetite but interest in food. Medications: Cerenia, Zofran (Ondansetron), Reglan (Metoclopramide)
- Vomiting: This may occur, but is usually self-limiting. Typically, this will resolve after 1-3 episodes. Medications: Cerenia, Zofran (Ondansetron), Reglan (Metoclopramide)
- Loss of Appetite: This is typically transient and is usually accompanied with other gastrointestinal signs (ie nausea). Sometimes this can also be due to the tumor itself. Medications used to manage this include those used for nausea and vomiting (see above) as well as mirtazapine or cyproheptadine.
- Diarrhea: If your pet develops diarrhea, we can prescribe a medication to address this. Again, this is commonly transient, and should only last for 24-48 hours. Occasionally, this can be accompanied by signs of frank blood, mucous and staining that are consistent with colitis. Medications used to manage diarrhea include Flagyl (Metronidazole), Tylan (Tylsoin), Probiotics (FortiFlora, Propectalin) and increased fiber in the diet (ie sweet potato, pumpkin).
- Tissue Damage: If some chemotherapy agents (ie vinca drugs, Doxorubicin) leak outside the vein, sever tissue reactions can result and include pain/irritation at the injection site, redness, swelling, bruiding and in some cases, extensive tissue death.
- Allergic Reactions: This side effect is rare but can occur with certain chemotherapeutic agents (ie L-asparaginase, Doxorubicin). Pre-emptive therapy with Benadryl +/- steroids may be recommended.
- Heart (Cardiac) Damage: Some chemotherapy agents (ie doxorubicin), in some rare cases can cause irreversible damage to the heart muscle. This is typically a cumulative dose effect therefore we limit the maximum total dose that your pet receives or recommend a cardiac screening prior/during therapy if signs/concerns arise. Less than 5% of patients develop heart disease as a result of chemotherapy.
- Kidney (Renal) Damage: This side effect is species specific as well as drug specific (ie Cisplatin in dogs, Doxorubicin in cats: Carboplatin and oral non-steroidal anti-inflammatory drugs in both species). Routine evaluations of blood work as well as urine samples help for us to monitor for this toxicity.
- Hair Loss (Alopecia): Pets rarely lose their hair while undergoing chemotherapy, but if they do, they are not bothered by it. The pets most at risk are animals that have hair that continually grows (ie Poodles, Old English Sheepdogs). Cats may lose their whiskers, and occasionally patchy hair loss can also occur. Typically, if an animal loses his/her hair during treatment, it will grow back once treatment has been discontinued and in some cases, may be a different color or texture.
How Should You Take Care of Your Pet After their Chemotherapy Treatment to Make Sure That You, Your Family and your Other Pets are Safe?
After treatment, trace amounts of active chemotherapy can be excreted by the body through secretions (ie saliva, urine, feces). Health risks that may be linked to such trace exposures are likely most significant if repeated over long periods (months or years) and are not related to short term exposures. Some populations of people should exert greater precautions (pregnant women, children, the elderly and individuals who are immunosuppressed). We recommend that you take precautions to minimize direct contact with urine, vomit and feces from your pet while receiving chemotherapy. We also recommend the following safety tips:
- Wear gloves when handling all excrement or vomitus. Place the waste in a sealed trash bag and discard in appropriate disposal areas. Wash your hands with soap and water.
- If your pet receives a tablet formulation of chemotherapy (ie CCNU, Cytoxan, Leukeran) and vomiting has occurred within 4 hours of treatment, check to see if the tablet is readily identifiable and contact your pet’s oncologist for further instruction. Do not pick up the tablet without wearing gloves.
- If administering home chemotherapy (ie Leukeran, Cytoxan), study medications, or small molecule inhibitors (ie Palladia, Kinavet), always read the dosing and handling instructions prior to administration. Wear gloves and avoid direct contact with the medications. Wash your hands with soap and water.
- Walk your pet in areas of low traffic, especially avoiding areas where children and other pets may frequent. The trace amounts of chemotherapy in urine and feces will break down spontaneously in the environment and does not pose an environmental risk.
- It is reasonable to minimize the opportunities for your pet to excessively lick you, your children and family immediately after treatment.
- Allow your pet the opportunity to have free access to water and frequent walks to use the restroom in order to minimize risk of accidents in the house.
- You do NOT need to have separate feeding bowls, water bowls, bedding or litter boxes for your other pets as long as these are well maintained and have not been soiled by the pet undergoing treatment.
Handling Chemotherapy
Whether your pet receives oral or intravenous chemotherapy in hospital, or you give oral chemotherapy at home, there are necessary precautions we recommend taking.
HANDLING:
- Store oral chemotherapy in an elevated and safe place away from children and pets.
- Avoid preparing chemotherapy in areas with food.
- Administer somewhere away from food and from soft, absorbent furnishings to be easily cleaned if there is a spill (e.g. a bathroom).
- Wear gloves when handling any chemotherapy or waste.
- Do NOT cut pills in half or open capsules.
The chemotherapy drug your pet is receiving is excreted through urine and feces, and present in vomit for up to 72 hours post-administration. Therefore, due to their cytotoxic properties, we recommend limiting contact with these fluids by following these simple guidelines.
CLEANING:
- Wear gloves when cleaning vomit.
- Wear gloves when cleaning urine or feces from the litter box, kennel, and outdoors.
- If possible, separate your cat’s litterbox from the other cats in the household for at least 72 hours. If not possible then be sure to scoop the litter box multiple times per day for those first 72 hours after receiving chemotherapy.
- Walk your pet away from high traffic areas and pick up feces to discard in a tightly closed bag in a waste receptacle.
- If walked in a high traffic area dilute area of urination with water.
- If your pet has an “accident,” remove solid waste and any possible liquid waste, and rinse the area with water. Then wash the area with a soap or bleach solution, followed by a second rinsing with water.
- If there is a chemotherapy spill (such as an open capsule) wipe with alcohol, then rinse with water, followed by cleaning with a detergent, and by rinsing with water.
- Soiled laundry should be washed separately with bleach prior to adding to routine laundry.
*Owners who are immunosuppressed and women who are pregnant, trying to conceive, or nursing should avoid handling urine, feces, cleaning the litter box, or other materials that have been contaminated.
EDITED & COMPILED BY :DR. ROHITRAJ,CANINE CONSULTANT,KLKATA
REFERENCE-ON REQUEST
https://www.pashudhanpraharee.com/neoplasm-in-a-dog/
https://www.msdvetmanual.com/special-pet-topics/cancer-and-tumors/cancer-treatment