Epidemiology, Treatment and Control of Theileriosis in Cattle
Dr. Pankaj Kumar1, Dr. Anil Kumar2, Dr. R.K. Sharma1, Dr. Sudha Kumari3
& Dr. Archana Kumari4
1- Associate Professor Veterinary Parasitology, BVC, BASU, Patna – 800014.
2- Associate Professor Veterinary Medicine, BVC, BASU, Patna – 800014.
3- Associate Professor Veterinary Microbiology, BVC, BASU, Patna – 800014.
4- Associate Professor Veterinary Surgery & Radiology, BVC, BASU, Patna – 800014.
Introduction
Theileriosis is a tick-borne infections disease of characterized by fever, anemia and disorder of respiratory and digestive tracks. In India, the disease in cattle is known as “Bovine Tropical Theileriosis”. In many respects Theileriosis is like Malaria in human beings and so it is also called malaria.
This disease was though recognized in India in 1905 (by Lingard), but its real impact was seen only in mid 1960 when exotic breeds of cattle were imported in large numbers for cross-breedings in Indigenous cattle to increase the milk production. It has become a disease of economic importance due to high degree of morbidity, mortality and prolonged convalescent period.
Etiology:
The disease is caused by Theileria annulata (a blood protozoan parasite) which is transmitted to cattle by the bite of ticks of genus Hyalomma, the most potent of which is Hyalomma anatolicum (three host tick).
Epidemiology:
All the age groups of cross-bred cattle are highly susceptible to Theileria annulata infection. The severity of the disease is more in young cross-bred calves with very high mortality rate. Clinical Theileriosis has also been observed in young indigenious calf. The adult indigenous cattle generally suffer from subclinical infection. But they become potent source of spreading the infection to other healthy cattle through ticks. The clinical cases in Indian buffaloes have rarely been reported. They are considered to be the carriers of Theileria organisms. The occurrence of the disease has been seasonal i.e. in summer and rainy months, which may be due to enhanced activity of vector ticks. The stress factors like hot and humid weather, transportation, malnutrition, pregnancy, lactation and even vaccination precipitate the occurrence of disease. The mortality is variable according to the severity of disease. It has been reported to be as high as 90%.
Clinical Symptoms:
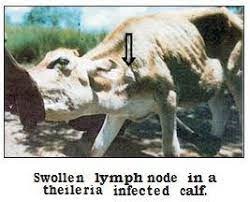
The first symptom is enlargement of superficial lymph glands(Fig-1) which develops within 8-12 days
Fig.-1. Enlargement of superficial lymph glands
(incubation period) after the bite of Theleria infected Hyalomma ticks. This symptom is mostly observed in the prescapular lymph gland and occasionally in the parotid lymph gland. The fever develops at this stage and the body temperature rises from 1030 to 1070 F. There is short sporadic cough, labored breathing, mucous discharge from eyes and nostrils and depraved appetite. The lungs become filled with fluid and the alimentary canal particularly the abomasum develops ulcers. The abortion may occur in pregnant cows.
Severe form of anemia develops causing marked reduction in the values of haemooglobin (Hb), packed cell volume (PCV) and total erythrocytic count (TEC). In the later stage of disease, the animal develops jaundice. The conjunctiva may become icteric. Diarrhoea also occurs in the last stage with faeces containing blood-tinge. The animal becomes weak and emaciated followed by death in 80-100% of cases. The course of the disease is 6-19 days with an average of 12 days in fatal cases. In mild form of the disease, the course is 22-23 days.
Sometimes unusual symptoms are also observed like swelling of eyes with protrusion of eyeballs form the socket leading to conjunctivitis, ulceration and opacity of cornea. These symptoms are generally seen in young calves. Nervous symptoms are found in cerebral form of Theileriosis. Cutaneous lesions showing urticarial growths have also been observed occasionally.
Post-mortem Findings:
The important P.M. findings consist of punched necrotic ulcers in the abomasum and occasionally in the small and large intestines and congestion and oedema of lungs. The punched necrotic ulcers in the abomasum are characteristic P.M. lesions and of diagnostic significance.
Diagnosis:
The diagnosis of the disease is based on the clinical symptoms and demonstration of parasites in the lymphnode biosy smears and peripheral blood smears after staining them with Giemsa’s or Leishman’s stain. At the initial stage of the disease, the schizont stage of the parasite is detected in the stained lymph node biopsy smears which appear in the cytoplasm of the lymphocytes.
In the later stage of the disease, piroplasm stage develop in the R.B.Cs. the piroplasms appear in the stained blood-smears in R.B.Cs. as a ring or oval shaped organisms either singly or in pairs. In heavy infection, the parasite may be 4-6 in number in one R.B.C . For the diagnosis of subclinical cases, serological tests are used.
Treatment:
The drug of choice is “Buparvaquone” marketed as Butalex/zubion. A single injection of Butalex /zubion at the dose rate of 1 ml./20 kg. body wt. i/m is usually sufficient, but in some cased, a second injection may be required within 72 hours of 1st injection. Not more than 10 ml should be injected at one site. Milk from lactating animal should not be used for 2 days following the treatment for human consumption. Butalex /Zuubion is effective against both schizont and piroplasm stages of Theileria annulata. Since, it is very costly drug, it is desirable to use after the confirmation of diagnosis.
In the absence of Buparvaquone (Butalex Zuubion) drug combinations consisting of antibiotic (Oxytetracycline), anti-blood protozoal (Dimenazene – Diaceturate) including antimalarial like Chloroquine (Nivaquine) may be used. Oxytetra cycline is used at the dose rate of 5-10 mg/kg body wt i/m for 5 days.
Long acting Oxytetracycline may be used in place of Buparvaquone at the dose rate of 20 mg/kg body wt i/m and to be repeated after 72 hrs. on 2-3 occasions. Diminazene-Diaceturate (Berenil/ Nilbery/ Prozomin) is used at the dose rae of 10-15 mg/kg body wt deep i/m on 2-3 occasions at the interval of 48 hrs.
Oxytetracycline has effect on schizonts, whereas Diminazene and Chloroquine have effect on piroplasms. Antipyretics like Paracetamol or Meloxicam may be used to reduce fever, Antihistaminics (Avil/Cadistion) should be given to prevent the reactions of Oxytetracecycline and Diminazene-diaceturate if any.
The supportive therapy consists of haematinics, such as Vit. B-Complex, Liver extract and Iron Preparations parenterally in required doses to overcome anaemia. In severly anaemic cases, when the haemoglobin level comes down to 3-4 g/100ml of blood, in that case blood transfusion may be of much value. For this, blood is collected from the Jugular vein of normally healthy cattle in to a sterilized empty glucose saline bottle containing anticoagulant solution sodium-citrate 3.85% at the rate of 10 ml for each 100ml of blood, the blood is transferred immediately to sick animal by slow drop method. 400-500 ml of blood can be transferred at a time. No cross-matching may be needed to determine the compatibility. For this, a small amount of blood (50-100ml) should be injected at first and the animal should be observed for half an hour, if no transfusion reaction occurs, the rest of the blood can be injected slowly.
Control:
The control measures consist mainly of two methods-
(1) Control of vector ticks
(2) Immunization of susceptible animals.
For the control of vector ticks, ectoparasiticides viz. Deltamethirin / Cypermethin (Butox/Clinar) are used effectively as spray in the required concentration. The spraying should also be done on the floor of animal shed including the crevices in the walls where ticks generally hide.
For immunization, schizont vaccine has been developed which is lymphoid cells grown schizonts attenuated after passages. But this vaccine has not become popular due to certain limitations. However, there is need for the development of safe and effective vaccine which can be used in all age group of susceptible cattle including the young calves producing longer immunity.