FOOD –BORNE ZOONOSES ( FBZs) & CONTROL STRATEGIES IN INDIA
Compiled & Shared by-DR. RAJESH KR. SINGH,LIVESTOCK CONSULTANT, JAMSHEDPUR, JHARKHAND,9431309542
rajeshsinghvet@gmail.com
Food-borne zoonoses (FBZs) are diseases transmissible from animals to man via the medium of foods derived from animals such as meat, poultry, fish and shellfish, milk and food by-products. The total number of people affected (at least 17 million worldwide each year) and the harm caused by FBZs make them a serious public health concern. Food-borne in toxication and food-borne infection emphasize the inextricable link between animal and human health activities that share the common ultimate goal of protecting, promoting, and improving the health and well-being of human populations. Food handlers and consumers should be made aware of the dangers of and the methods of reducing the risk from zoonoses.
Food-borne diseases, including food-borne intoxications and food-borne infections, are terms applied to illnesses acquired through consumption of contaminated food, and are also frequently referred to as food poisoning. Worldwide, food-borne diseases are a major health burden leading to high morbidity and mortality. In India, the burden of food-borne disease is not known. Most food-borne diseases go unreported, only few are reported by the media, usually those with high morbidity and/or occurring in urban areas.
Estimates suggest that almost half of the population of
the world is affected by water-borne and food-borne infections.
Food-borne zoonoses are defined as ‘those diseases contracted
from eating foods of animal origin’ such as milk, meat and
eggs. This is a broad definition and covers a wide spectrum of
pathogens such as bacteria, viruses, and parasites, although the
most important on a day-to-day basis are mainly bacteria.
Food-borne zoonoses are an important food safety issue
worldwide and have also become an important cause of
decreased economic productivity in both developed as well as
developing countries. Rapid industrialization, change in food
preferences and food habits, mass food processing and lack of
effective food quality control system has led to the emergence
of many food-borne pathogens. More than 250 known diseases
are transmitted to humans through food.
Food producing animals (cattle, sheep, goats, pigs,
chickens and turkeys) and their products are the major sources
for many of zoonotic organisms, which include Salmonella
spp.,Campylobacter spp., Listeria monocytogenes, Escherichia
coli, Yersinia enterocolitica, Clostridium spp., Brucella spp.,
Staphylococcus aureus, Vibrio spp., Aeromonas spp., etc. as
well as food-borne viruses namely Norwalk and rotaviruses
along with some food-borne parasites such as Toxoplasma,Sarcocystis, Cryptosporidium, Trichinella, Taenia, Diphylobothrium etc. These organisms can contaminate animal/poultry carcasses at slaughter or cross-contaminate
other food items, leading to human illness and cause huge
economic losses.
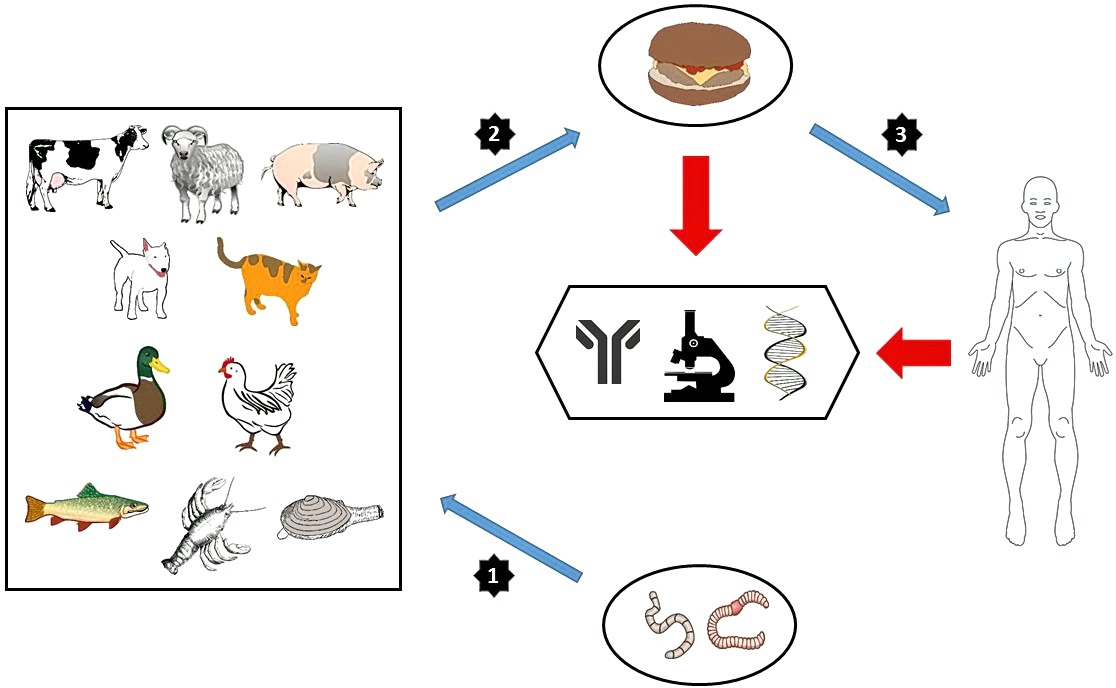
Typical transmission pathway
An animal suffering from a disease, which may not be apparent, creates a product of either milk or body tissue in which the causative organism is present. This product is either further processed or directly passed to a final consumer who then either with or without cooking eats the contaminated item, and in susceptible cases develops the disease after a variable incubation period.
Some of the important food-borne bacterial zoonoses
In many countries of the world, bacterial food-borne
zoonotic infections are the most common cause of human
intestinal disease. Salmonella and Campylobacter account for
over 90 % of all reported cases of bacteria-related food
poisoning world-wide. Poultry and poultry products have been
incriminated in the majority of traceable food-borne illnesses
caused by these bacteria, although all domestic livestock are
reservoirs of infection. Other important bacterial zoonoses are
cause by Listeria monocytogenes, Escherichia coli, Yersinia enterocolitica, Clostridium spp., Brucella spp., Myocobactreium spp., etc. Some of these important food-borne bacterial zoonoses are described as follows:
Salmonella
Salmonella infections are prevalent all over the world
among various species of domestic as well as wild animals
besides poultry, ducks, birds, amphibians, reptiles and rodents.
More than 2541 serovars of Salmonella are identified so far.
Salmonellosis caused by non-typhoidal species is not only
more prevalent but has also shown an increasing trend world
over with majority of cases being caused by S. Enteritidis and
- Typhimurium. In India, human salmonellosis is endemic and
one of the most widespread zoonosis. Salmonella organism has
been isolated from a variety of foods including pork and pork
products, beef, chevon, mutton, fish, milk and its products,
fruit juice, fruits and vegetables and egg shells. Animals may
be asymptomatic carriers of Salmonella. They may also suffer
clinical disease with intestinal disturbance, septicaemia and
death. Transmission usually follows ingestion of infected food,
or direct or indirect contact with animal faecal material. In humans symptoms include sickness, diarrhoea, abdominal pain and fever. The most significant serotype in terms of mortality is S. typhimurium DT104, which shows a 3% mortality rate, being multi-drug resistant to many of the antibiotics.
Campylobacter
Campylobacter are a major cause of gastroenteritis
throughout the world. This particular pathogen is widespread
and present in many farm animals. In particular, poultry are
very susceptible to heavy bacterial loading. Under normal
circumstances, the animals show no sign of disease, although
there have been cases of abortion in sheep being linked to C.
jejuni. The bacterium has been isolated from pigs, birds, cattle,
dogs, cats, unpasteurized milk and water supplies. Infection
occurs mainly following consumption of faecal contaminated
undercooked carcasses especially poultry, or of milk. The
organism is capable of surviving freezing and has been shown
to survive for several months in frozen poultry, minced meat
and certain chilled foods. The most common symptoms of
Campylobacter infection include diarrhoea, abdominal pain,
fever, headache, nausea and vomiting. Symptoms usually start
2-5 days after infection, and last for 3-6 days. Severe
complications, such as Guillain-Barre syndrome, may
followCampylobacter infection.
Listeria
- monocytogenes is considered emerging because the
role of food in its transmission has only recently been
recognized. The disease is most often associated with
consumption of foods such as soft cheese and processed meat
products that are kept refrigerated for a long time because
Listeria can grow at low temperatures. Outbreaks of listeriosis
have been reported from many countries. Several outbreaks of
listeriosis associated with consumption of milk and dairy
products have occurred in India. It has been isolated from the
milk of cow, buffalo and goat in India. It has also been reported
from Seafood, beef, raw milk, vegetables and fresh raw fish.
Animals can carry the bacterium without appearing ill and can
contaminate foods of animal origin, such as meats and dairy
products. Unpasteurised (raw) milk or milk products made from unpasteurized milk may contain the bacterium. In most cases, infection occurs following ingestion of contaminated foodstuffs. Clinical onset usually follows fever, headache,
nausea and vomiting, and symptoms similar to a severe chill.
Abdominal cramps, stiffness of the neck and photophobia may
also be present. The condition may progress with organ
involvement, including endocarditis, internal lesions, metritis,
septicaemia and meningitis. Focal necrosis in the placenta may
occur with spontaneous abortion, premature birth or infective
transfer to the baby at birth. A fatality rate of higher than 20%
of clinical cases has been seen when treatment is not made, or
is not started quickly.
Escherichia coli
coli forms a part of most mammalian bacterial gut flora. It has a vast array of serotypes: some are benign, whereas others are dramatically pathogenic. This can vary from species to species; a benign form in one animal may be a deadly organism in another. The particular serotype of major concern is O157:H7, which was first identified as a major cause of serious outbreaks of food poisoning. This serotype is variously known as entero-haemorrhagic E. coli (EHEC), shiga toxin-producing E. coli (STEC) or verocytotoxin-producing E. coli (VTEC) O157. Many outbreaks and sporadic cases have been reported due to STEC in developed as well as developing countries. It is transmitted to humans primarily through consumption of contaminated foods, such as raw or undercooked ground meat products and raw milk. Symptoms of the diseases caused by EHEC include abdominal cramps, haemorrhagic colitis, haemolytic uraemic syndrome etc. The National Salmonella and Escherichia Centre, Kasauli conducted an epidemiological survey of E. coli O157 in different regions of India during the 10-year period (Seghal et al., 2008), in which a significantly high percentage of E. coli O157 was isolated from meat, milk and milk products, seafood and water.
Yersinia enterocolitica
Of the same bacterial genus as plague, it is transmitted
to humans by ingestion of foods as diverse as meat (pork, beef
and lamb), oysters, fish and raw milk. It causes acute-onset of
gastroenteritis with diarrhoea and vomiting, marked fever and
abdominal pain. The pain can be so severe that it mimics
appendicitis and has also led to misdiagnosis of Crohn’s
disease. It is capable of producing clinical complications which
include septic arthritis, colonisation of existing wounds,
bacteraemia and urinary tract infections. Luckily it is rarely
fatal.
Clostridium spp.
Clostridium perfringens, the causative anaerobic
bacterium of many cases of gas gangrene, may also cause a
food-borne disease. Widespread in the environment, and an
inhabitant of the gastrointestinal tracts of humans and animals,
it is often found in foodstuffs as a result of faecal
contamination. As with other forms of clostridial diseases, it is
the production of exotoxins by the pathogen that causes the
main damage, especially where the ingested food carries a
large inoculum, or heavy toxin load. The usual pattern of
disease is linked to the ingestion of a number of viable C.
perfringens organisms that may produce clinical symptoms of
abdominal cramps, diarrhoea and fever.
Botulism as a complex of disease state arises from
contact with C. botulinum or its associated neurotoxin. There
are seven types of botulism toxin associated with the bacteria,
designated by the letters A-G. Only the A, B, E and F toxins
are known to cause illness in humans. Often associated with
ducks, geese and some other types of poultry, it can also be
found in cattle and horses, which can act as hosts and
amplifiers for some strains. The disease usually begins 18-36
hours after the ingestion of the toxin. Early signs include gait
difficulties, dysphagia and impaired vision. Respiratory
distress, muscle weakness, and abdominal distension and
constipation may appear progressively.
Brucella
Brucellosis is a widely prevalent and economically very
important bacterial disease caused by Brucella species, of
which B. abortus and B. melitensis are the main causes of
occupational zoonosis in farmers, veterinarians and workers in
meat industry. It is common in organized herds and in areas
with high rainfall and humidity. Source of infection in human
is through the drinking of infected raw milk or unpasteurized
milk, handling of aborted foetus, fluids and foetal membranes,
slaughter house workers and butchers contract infection while
handling foetuses, after births or by contact with vaginal
secretions, veterinarian gets infection during rectal examination
without wearing gloves and while conducting post mortem
examination, through skin abrasions and conjunctiva. There are
losses due to abortion in the affected animal population, loss of
progeny and reduced milk production. In humans disease is
clinically characterized by chills, profuse sweating, weakness
and fatigue, insomnia, sexual impotence, headache, arthralgia
and generalized malaise, which last for weeks and months;
commonly shows remissions (hence also known as undulant
fever).
Mycobacterium
Tuberculosis caused by Mycobacterium bovis needs no introduction. Human-to-human spread of resistant serotypes of M. tuberculosisis now more significant than the bovine form acquired from dairy products. Ingestion and inhalation are the most common mode of transmission. Consumption of infected milk and milk products is the mode by which food borne zoonoses occur. It is a chronic disease of man and animals causing development of tubercle in vital organs. The pulmonary tuberculosis is the most common form, characterized by cough, fever, fatigue, weight loss, chest pain and night sweat in human beings.
Some of the important food-borne viral zoonoses
Numerous viruses can be found in the nature, but only a few are commonly recognised as important food borne pathogens. These can be classified into three main groups, according to the type of illness they produce:
Viruses that cause gastroenteritis such as Norovirus, Enteric adenovirus (types 40/41), Rotavirus (group A -C), Sapovirus, Astrovirus, Coronavirus. Enterically transmitted hepatitis viruses (Hepatitis Aand E); andA third group of viruses that replicate in the human intestine but cause illness after they migrate to other organs, such as the central nervous system or the liver such as Enteroviruses.
Food borne illness has been documented for most of these
viruses, but recent studies show that the Noroviruses (NoV)
and hepatitis A virus (HAV) are by far the most common cause
of illness by this mode of transmission. Some large food borne
outbreaks have occurred with group B and C, rotaviruses, and
waterborne outbreaks have occurred with hepatitis E virus.
These viruses are spread by the faecal-oral route, cross-
contamination and infected food handlers. Rotaviruses,
classified in the reoviridae family, are ubiquitous and have
been isolated from a variety of mammalian species. Rotavirus
has been recognized as one of the most common cause of
severe gastroenteritis in a wide variety of animal species
including children, calves and piglets worldwide.
Outbreaks of rotaviral gastroenteritis are frequently observed in
institutional settings such as hospitals, nursing homes, day-care
centers, and schools. The incidence is higher during winter
season in temperate climate whereas, no seasonal variations for
tropical countries. However, certain studies reported higher
incidence during rainy season. In developing countries,
Norwalk viruses are so common that a very high percentage of
children develop immunity at an early age. Generally the
illness that results from Norwalk viruses is mild and brief.
Foods are contaminated with Norwalk viruses via the faecal-
oral route and contaminated water. Salads, insufficiently cooked clams and oysters, ice and water are the most commonly implicated foods. Common symptoms in viral food borne zoonoses include nausea, vomiting, diarrhea, abdominal
cramps, headache, fever/chills, muscle aches. Symptoms
usually last 1 or 2 days. However, during that brief period,
people can feel very ill and vomit, often violently and without
warning, many times a day.
Some of the important food-borne parasitic zoonoses
Food-borne parasitic zoonoses cause death and serious
diseases in humans and animals worldwide, and are of both
public health significance and socioeconomic importance.
Food borne parasitic infections have been recently identified as
an important public health problem having considerable
economic impact in terms of morbidity, loss of productivity
and health care costs. Poor sanitation and traditional methods
of food preparation accelerated the spread of food borne
parasitic infections. Some of the important food-borne parasitic
zoonoses are described as follows:
Toxoplasmosis
Toxoplasma gondii is possibly the most wide spread
and prevalent protozoan parasite on earth, infecting
approximately half a billion people. Toxoplasma gondii is a
parasite of domestic and wild cats that potentially is capable of
infecting all vertebrates. Toxoplasmosis can be transmitted to
humans via several routes. Although a major source of
infection is thought to result from contamination of the
environment with oocysts shed in cat faeces. Transmission of
T.gondii by ingestion of tissue cysts in raw or under cooked meat from a variety of livestock and game animals has been documented as another major source of human infection. It is characterized by retinochoroiditis and encephalitis, and abortion in pregnant women (especially at first trimester). In animals, it causes abortion especially in sheep.
Sarcocystosis
Sarcocystis spp., like T .gondii, is coccidian protozoan
which have a global distribution. Humans acquire S. hominis
by consumption of uncooked beef containing zoitocysts.
Sarcocystis hominis is only mildly pathogenic in humans,
causing stomach pains, nausea and diarrhoea; Sporocysts begin
to be passed in the faeces after 14 to 18 days (11 to 13 days
after infection with S. suihominis). Sarcocystis suihominis is
acquired by eating zoitocysts in under cooked pork. Sarcocystis
suihominis is more pathogenic than S. hominis, causing
stomach pains, nausea, diarrhoea and dyspnoea within 24 hours
of infection.
Cryptosporidiosis
Cryptosporidium spp. are spore-forming parasitic
protozoans found widely in the environment in an extensive
variety of foodstuffs, including salad and vegetables, raw meat
and meat products, offal and milk, usually associated with
contamination arising from animal faecal matter.
Cryptosporidium parvum is considered to be a particularly
significant pathogen. Calves, lambs and deer have been
identified as asymptomatic animal reservoirs, capable of
shedding viable organisms in their faeces. Human infection
follows either direct contact with animal faeces or consumption
of inadequately cleaned or cooked products. Following a pre-
patent period of between 2 and 14 days and in individuals with
no underlying risk factors, there is profuse self-limiting watery
diarrhoea, with abdominal pain and cramps, and a low fever
that may last up to 7 days.
Taeniosis or Cysticercosis
Taenia solium (tapeworm of pigs) and T. Saginata
(tapeworm of cattle) have cosmopolitan distributions with the
former being more widespread in the rural areas of Latin
America, Africa and Asia. Cysticercisis is caused by the
intermediate stages of the tape worms Taenia solium and
Taenia saginata. It is clinically characterized by abdominal
pain, anorexia, nausea, diarrhoea and constipation, loss of body weight and debility. Nervousness and insomnia may also occur.
Human beings are universally susceptible to taeniosis.
Infection is more common in low socio-economic group of the
people. Larvae (Cysticercus cellulosae – measly pork) and
(Cysticercus bovis – measly beef) fully develop in the different
predilection sites, such as heart, diaphragm, internal masseter,
tongue, neck, intercostals and abdominal muscles, less
commonly brain, liver, lung, kidney and eye after reaching to
the blood by penetrating the intestinal wall when infected eggs
are consumed. This is the infective stage for human beings.
Man gets infection by ingesting measly beef or pork
undercooked. Cysticercosis is more serious than taeniosis in
humans. It recognized as:
Myocysticercosis:
Muscular cramps, pain and muscle fatigue.
Ocular cysticercosis: Presence of cysticerci in vitreous humor and anterior chamber of eyes leads to uveitis, iritis, retinitis and palbebral conjunctivitis.
Neurocysticercosis: Signs depend on the location of the cyst found on the brain. Usually it found in the meninges, cerebral cortex and ventricles. So, symptoms
of meningitis, epileptic encephalitis, headache, ataxia, nausea, vomiting and visual disturbances may be observed.
Trichinellosis
It is a type of food-borne helminthosis, caused by Trichinella spiralis. Trichinellosis can occur where humans eat raw or improperly cooked meat or meat products from infected pigs, wild boars, horses, walruses, dogs and many other domestic or wild mammals. Number of larvae ingested by humans determines the clinical disease. Usually 10 to 100
parasites per gram of muscle cause clinical signs. It is clinically characterized muscle soreness and pain due to irritation, enteritis, edema of upper eyelids, thirst, profuse sweating, chills and eosinophilia, and eventually, death due to myocardial and respiratory failure may occur.
Control strategies
Control of food borne disease is a multifaceted process,
as there are no vaccines available for most food borne
pathogens. The prevention of infection requires control
measures at all stages of the food chain, from agricultural
production on the farm to processing, manufacturing and
preparation of foods in both commercial establishments and the
domestic environment. The general strategy of control is to
understand the mechanisms by which contamination and
disease transmission can occur well enough to interrupt them.
Increasing liberalization of trade, and increasing competition in
the international market place, have meant that live animals,
animal feed, food ingredients and products are now sourced on
a global stage, affording the opportunity for zoonotic
pathogens to be disseminated widely. The public health
veterinarian needs to be proficient in setting up surveillance
systems to monitor trends, establish priorities, inform policy-
makers and control interventions. Understanding the likely
routes of infection and the life cycle of the pathogen allows
selective measures to be applied in a focused way, breaking the
transmission route at its weakest point. Different basic steps to
prevent the occurrence of these food borne infections are
discussed below.
Step 1: Control the disease in the animals
The effective control in the food chain requires the
incidence of infection in animals to be reduced. The health of
consumers is inextricably linked to the health of food
producing animals and the importance of herd and flock health
cannot be underestimated. The incidence of zoonotic disease in
animals may be reduced by the use of vaccination, clean
foodstuffs and water, and good housing and husbandry
practices. Overcrowded or unsanitary conditions can often lead
to overt disease or unthrifty animals, requiring more
therapeutic support for them to maintain sufficient health to
attain slaughter weight or to continue to be productive. A reduction in infection rates has a dramatic effect on the incidence of infection further down the food or product chain. The associated lower levels of contamination produce a lower likelihood of illness.
Step 2: Reduce contamination at harvesting
When eggs are picked out, or cows milked, the
application of sensible hygiene precautions is essential. Eggs
should be free of droppings and cleaned and date marked. In
dairies, the udder of the cow and the milking machinery should
be as clean and hygienic as possible, with subsequent
disinfection after each milking. Pipe work and items such as
clusters should be maintained and replaced as necessary to
maintain adequate operating parameters. Milk should pass to a
bulk tank and be subsequently chilled rapidly for later transport
and pasteurization. At abattoirs, tight veterinary inspection
both pre- and post-slaughter must be practiced. Animals that
display heavy faecal contamination should be cleaned or
rejected. Slaughterhouse controls should prevent or reduce
onward transmission into the food chain, with rejection of
suspect carcasses. Prompt refrigeration of meat and careful
cleaning of the carcass can reduce bacterial contamination
drastically.
Step 3: Retailing controls
Disinfection of working tools and areas, along with
personal and premises hygiene procedures protect consumers
and workers from zoonotic infection. Sourcing products from
assured suppliers, temperature and environmental monitoring,
and the separation of cooked and raw products reduce the
possibility of amplification and transmission of infection. The
tight control of ‘use-by’ and ‘sell-by’ dates is mandatory, as is
periodic inspection by public health officials, and the
implementation of monitoring of refrigeration and freezer
plants.
Step 4: Domestic precautions
In the home, consumers should use common-sense measures, including disinfection of surfaces and equipment, personal hygiene procedures and thorough appropriate cooking techniques. Using a refrigerator correctly and observing sell-by dates would prevent many cases of food poisoning.
There are several factors that continually contribute to the occurrence of outbreaks of food-borne disease and often several of these occur simultaneously, thus amplifying outbreaks. These factors include: contaminated raw ingredients (including water), inadequate refrigeration or storage, insufficient cooking, cross-contamination between raw and cooked food, poor personal hygiene of staff, poor general hygiene on premises, and untrained staff. Robust food safety management systems with adequate process controls are essential with good manufacturing practice and hazard analysis and critical control points (HACCP). Prior to establishing HACCP, good food hygiene standards must already be in place, particularly in the following areas:
Infrastructural and equipment requirements.
Food safety specifications for raw materials.
The safe handling of food (including packaging and transport).
Sanitation (cleaning and disinfection). Water quality.
Maintenance of the cold chain. The health of staff.
Personal hygiene. Training.
Food waste handling. Pest control.
These standards are designed to control hazards in a general way and they are clearly prescribed in the Codex Alimentarius.
Principles of Hazard Analysis and Critical Control Point (HACCP)–——–
- Analyse hazards – Potential hazards associated with a food and measures to control those hazards (biological, e.g. a microbe; chemical, e.g. a toxin; or physical, e.g. ground glass or metal fragments) are identified.
- Identify critical control points – These are points in a food’s production – from its raw state through processing and shipping to consumption by the consumer – at which the potential hazard can be controlled or eliminated. Examples are cooking, cooling, packaging, and metal detection.
- Establish preventive measures with critical limits for each control point – For a cooked food, for example, this might include setting the minimum cooking temperature and time required to ensure the elimination of any harmful microbes.
- Establish procedures to monitor the critical control points – Such procedures include determining how and who should monitor the cooking time and temperature.
- Establish corrective actions when monitoring shows that a critical limit has not been met – For example, reprocessing or disposing of food if the minimum cooking temperature is not met.
- Establish procedures to verify that the system is working properly – For example, testing timeand-temperature recording devices to verify that a cooking unit is working properly.
- Establish effective record keeping for documentation – This would include records of hazards and their control methods, monitoring of safety requirements and action taken to correct potential problems.
Five Keys to Safer Food
- Keep Clean Wash your hands before handling food and often during food preparation
- Wash your hands after going to the toilet
- Wash and sanitize all surfaces and equipment used for food preparation
- Protect kitchen areas and food from insects, pests and other animals§
- Separate raw and cooked food Separate raw meat, poultry and seafood from other foods
- Use separate utensils such as knives and cutting boards for handling raw foods
- Store food in containers to avoid contact between raw and prepared foods§
- Cook thoroughly Cook food thoroughly, especially meat, poultry, eggs and seafood
- Bring foods like soups and stews to boiling to make sure that they have reached 70°C
- Reheat cooked food thoroughly§
- Keep food at safe temperatures Do not leave cooked food at room temperature for more than 2 hours
- Refrigerate promptly all cooked and perishable food (preferably below 5°C)
- Keep cooked food piping hot (more than 60°C) prior to serving
- Do not store food too long even in the refrigerator
- Do not thaw frozen food at room temperature§
- Use safe water and raw materials Use safe water or treat it to make it safe
- Select fresh and wholesome foods
- Choose foods processed for safety, such as pasteurized milk
- Wash fruits and vegetables, especially if eaten raw
- Do not use food beyond its expiry date§
Conclusions
Food-borne zoonotic diseases are caused by consuming food or drinking water contaminated by pathogenic (disease- causing) micro-organisms such as bacteria and their toxins, viruses and parasites. They enter the body through the gastrointestinal tract where the first symptoms often occur. The risks of contamination are present from farm to fork and require prevention and control throughout the food chain. To protect consumers from these food-borne zoonoses, an integrated approach to food safety from the farm to the fork is needed to be adopted.
References: -On request-