GLANDERS-(FARCY) OUTBREAK & PROTOCOLS FOR NOTIFICATION & SURVEILLANCE IN INDIA
by-DR RAJESH KUMAR SINGH ,JAMSHEDPUR,JHARKHAND, INDIA, 9431309542,rajeshsinghvet@gmail.com
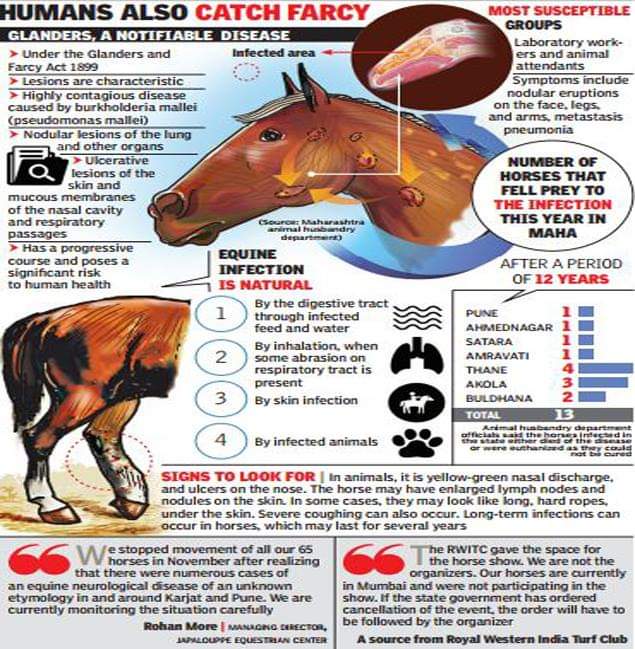
Glanders is an infectious, highly contagious and usually fatal disease
that is caused by the bacterium Burkholderia mallei. Glanders is primarily
a disease affecting horses. It also affects donkeys and mules and can be naturally
contracted by other mammals. This disease is characterized by serial development
of ulcerating nodules that are most commonly found in the upper respiratory tract,
lungs and skin. The disease is zoonotic and the organism is infectious for humans,
with a high fatality rate in untreated septicaemia cases. The causative organism is
present in nasal exudates and discharges from ulcerated skin of infected animals.
Clinical sign of Glanders are as follows:
After an incubation period of 3 days to 2 week, acutely affected animals
usually have septicaemia, high fever (as high as 106°F), weight loss and
subsequently, a thick, mucopurulent nasal discharge and respiratory signs. Three
forms i.e. Nasal, Pulmonary and Cuteneous forms of Glanders are recognized and
an animal may be affected by more than one form at a time. Inflammatory nodules
and ulcers develop in the nasal passages and give rise to a sticky yellow discharge.
Stellate scarring follows upon healing of the ulcers. The formation of nodular
abscesses in the lungs is accompanied by progressive debility, coughing and may
also be accompanied by diarrhoea. In the Cuteneous form along their course, which
then ulcerate and discharge yellow pus. Nodules are regularly found in the liver and
spleen, leading to wasting and death. Following steps are to be taken up for
minimizing the spread of disease.
Dos Do nots
1. Isolate the animal suspected for
showinq above symptoms Do not mix sick and healthy animals
2. Keep feeding and watering trough
separate for sick and healthy animals. Do not share feeding/watering troughs
between healthy and suspected sick
animals
3. Bury the left over feed/fodder rejected
by the sick animals Do not throw in open, the, left over feed
and fodder left by the sick animals.
4. Restrict the movement of sick animals Immediately move the sick animals to
designated isolated place.
5. Separate persons should handle sick
and healthy animals. Do not allow the same person to handle
sick and healthy animals.
6. wash your hands with soap and water
every time handling suspected
animals/feed fodder, water through, etc. Do not touch eatables without wasting
hands properly.
7. Recovered animals if any be kept
isolated till disposal. Do not mix up the recovered ponies with
the healthy stock.
8. Bury the dead animal deep
underground at the designated place. Do not open the carcases of dead
animals.
9. All sheds be disinfected with suitable
disinfectant. Do not keep healthy stock in sheds used
by sick animals.
10. Keep close watch for symptoms like Do not touch eyes/nasal/wound
nasal and eye discharges, respiratory discharges. These may contain disease
distress and skin sores. Bacterium
11. Personnel having wounds, scratches Do not handle animals if you have small
and abrasions on hands should never cuts or wounds on hands & arms.
handle sick animals
Destruction of the infected animal:
Carcasses of animals may be disposed of either by burial or burning
immediately to prevent the spread of the disease. If euthanasia is to be performed,
the use of Pentobarbital or a Pentobarbital combination or Magnesium Sulphate
could be used.
Burning is preferred, but method of burial could also be adopted. For burial, a suitable site away from streams, rivers, canals or other water supply is to be selected. A pit of minimum 8 ft. deep is to be made. The area requirement is about 3 Sq. Yards. The dead animal is put into the pit with feet upwards which are normally folded. The carcass is covered with quick lime followed by filling of the pit. The burial area is fenced so that stray dogs do not scavenge.
Disinfection of the premises: ———
All affected areas including stables, water and feeding trough, other
fittings are disinfected by use of blow lamps or by burning soiled hay and all
contaminated disposable equipments and other materials, should be disinfected by
using suitable disinfectants. Vacation of stables soon after the detection of first
Glander case should be adopted. Personnel in close contact with the diseased
animal should follow high standard of personal hygiene and strict antiseptic
measures.
Surveillance of disease:
Surveillance should aim at:
a) Detecting the foci of the disease and
b) Estimating rate of prevalence in a population.
Extensive surveillance by the Veterinary Surgeons in the various villages/ talukas/ districts of the State need to be carried in the States. The clinical cases affected and in contact equine should be segregated appropriately and dealt as per “The Prevention and Control of Infectious and Contagious Diseases In Animals Act, 2009”. Surveillance should include physical examination and sero testing depending upon the facilities available.
Advise for surveillance of in-contact animals
The in-contact animals should be kept under physical inspection and
sero surveillance for a period of two months. All positive reactors showing clinical
picture, positive on CF test need to be eliminated. The details of districts/Taluka
indicating the total strength of horses are to be prepared of the affected districts.
Mapping of routes of horses/equines around 25 kms. From the nuclei of infection is
to be worked out and on defined routes where movement of horses is in vogue need
to be monitored or clinical examination by Veterinary Surgeons. The topographical
details of districts need to be drawn and strength of horses/ equines is recorded.
a) Sampling of the in-contact animals is to be done as follows:
Horses/mule/donkeys I. 100% -5 km around the nuclei of infection
11. 20% -5 km above to 25 km. Around the nuclei
of infection
Through bred I. 100% related to all horse including race horses
irrespective of the distance in State
11. 100% in all orqanized equine establishment
Studs I. 100% yearlings and 100% foals
11. 20% mares and stallions at the Studs
b) Extensive physical surveillance of districts around 50 km from the
nuclei of infection is to be carried out.
Banning on movement:
Movement of all horses / equines is to be restricted for 3 months from
the last destruction of positive reactor horse. After 3 months based on physical
examination and serological test results, the need for restriction on further movement
of horses is to be decided by the State Department. If no case of Glanders is
reported after six months, movement can be allowed based on sero negativity by
complement fixation test. Restriction on movement should include restrictions on
animal fairs dealing in equines.
Procedure for declaration of freedom from disease:
OIE guidelines need to be adopted for this purpose. Clinical
examination / rising and failing titre by CFT be followed by the second test after one
month. If all the horses are found negative, another test should be done within three
months from the first testing. Minimum of three test in the first three months be
followed by another two test within next six months are to be conducted. If all the
tests are found negative, the outbreak could be considered free from infection.
Strategy for routine check up of horses:
Govt. Veterinary Hospitals in the State having reported isolated cases or sporadic outbreak of Glanders should be alerted for routine check-up for horses in the area. Suspicious case of Glanders based on clinical examination should take necessary steps for confirmation of the disease by the following agencies:
1. National Research Centre on Equines, Sirsa Road, Hisar.
2. Central Military Veterinary Laboratory, Meerut.
Samples to be collected for confirmation:
In general, following samples are to be collected and sent to laboratory for diagnosis of Glanders:-
i) Swabs of the exudates from the nostrils.
ii) Section of nodular lesions/ lymphnodes
iii) Air dried smears of exudates.
iv) A paired Serum samples.
Material is to be submitted to the State Disease Diagnostic Laboratory,
All the procedures/modalities as provided under “The Prevention and Control of Infectious and Contagious Diseases In Animals Act, 2009” shall be followed strictly.
Epidemiology
Glanders occurs rarely in humans and gets transmitted from infected animals by direct contact with body fluids through abrasions or cuts and mucosal surfaces such as nose and eyes. Symptoms include chest pain, muscle aches, swollen lymph nodes, fever with chills, cough, pulmonary abscesses, nasal discharge and septicemia.
Diagnosis of Glanders (Farcy) in Horses
The veterinarian will go over the medical history of the horse. The veterinarian will need to know what symptoms have you noticed, and when did they start. He will need to know if your horse has been in contact with other animals. The veterinarian will then perform a full physical examination. The horse’s physical exam may include: Listening to his heart, lungs and gastrointestinal tract with a stethoscope. Blood pressure Weight Rectal exam Checking the color of the gums Inspection of the sores and lesions Palpation of the limbs and muscles Palpation of lymph nodes Overall body condition of the horse
Diagnostic tests may include:
Complete blood count – Checks the count of platelets, red and white blood cells and helps determine if there is a bacterial infection Urinalysis – Checks for kidney function, crystals, blood or bacteria in the urine If the veterinarian suspects fluid in the lungs, chest x-rays will be recommended Take a culture from the lesion’s discharge Smears of the discharged examined under a microscope to confirm the bacteria Serological test can also confirm the bacteria.
Treatment of Glanders (Farcy) in Horses
Once Glanders is confirmed the horse must be quarantined. The bacteria can stay alive, with the right conditions, for up to one month. Stalls, water troughs, grooming tools, and saddles must be thoroughly disinfected and cleaned. Antibiotics will be prescribed to the horse. The disease may be resistant to particular antibiotics, so the use of several different medications may be required. Skin lesions and sores will need to be cleaned with an antiseptic. Medicated ointment will need to be administered to the sores. It is important for the person caring for the horse to use gloves, mask, and eye covering. If the horse was around other animals, they too should be tested for Glanders. The organism Burkholderia mallei primarily infects horses, donkeys and mules. It is not as common, but Glanders can also be transmitted to goats, cows, dogs and cats.
Recovery of Glanders (Farcy) in Horses
The disease is usually fatal in donkeys and mules but horses have a better prognosis. Antibiotic treatment is essential for the horse’s recovery. A follow-up visit will be needed to check on the horse’s progress. Diagnostic tests will need to be retaken. Unfortunately, some horses that do survive Glanders become carriers of the disease. This means that they can infect other animals and humans. In cases where the horse is diagnosed a carrier to the disease, he will need to live the rest of his life in quarantine. Anyone handling the horse will need to take safety precautions, such as gloves, mask or face shield. Horses are very social animals and living under quarantine will make the horse very depressed. The veterinarian may suggest euthanasia. Currently there is no vaccine against Glanders.
Biological warfare and bioterrorism of glanders:
Burkhoideria mallei are a group B biothreat agent and
are a host-adapted pathogen (Chandler and Landrigan,
2004). Due to the high mortality rate in humans and the small number of organisms required to establish infection, it is regarded as a potential biological warfare or bioterrorism agent along with closely related
B. pseudomallei, the causative agent of melioidosis.
During the 1st World War, large numbers of Russian
horses and mules on the Eastern Front was intentionally
infected with glanders by Germans (Wheelis, 1998;
Alibek and Handelman, 1999). This severely affected the troop and supply convoys, artillery movement which are dependent on horses and mules. Subsequently, the
human cases in Russia increased with the infections
during and after World War I (Bossi et al., 2004).
During World War II Japan intentionally infected
horses, civilians and prisoners of war with glanders at the
Pinfang Institute, China (Rega, 2007). In China, during
World War II, 30% of the tested horses were infected with glanders, but human cases were rare. The -U.S. studied this agent as a possible biological warfare weapon in 1943-44, but they did not weaponize it. The Soviet Union is also interested in glanders as a potential biological
warfare agent after World War II. If this organism is
aerosolized during a biological attack or in a laboratory accident, the morbidity rate could reach very high. Its use
as a biological weapon is now banned under the
international Convention on the Prohibition of the
Development, Production and Stockpiling of
Bacteriological and Toxin Weapons and on Their
Destruction (Rosebury and Kabat, 1947; Woods, 2005;
Wittig et al., 2006; Pawaiya and Chauhan, 2008).
PREVENTION AND CONTROL
No human or veterinary vaccines are available for
immunization/prevention of Glanders (Estes et al., 2010;
Burtnick et al., 2012). The immune evading strategy and genomic fluidity of this complex pathogen have made the use of live vaccine unsatisfactory (Nierman et al., 2004; Romero et al., 2006). Efforts need to be made for
identifying broadly protective antigens, efficient vaccine delivery/adjuvant systems and an exploring protection from both acute and chronic infections which would altogether pave way for the development of effective vaccine for B. mallei (Bondi and Goldberg, 2008).
Experimentally, two live attenuated strains of B. mallei, a capsule mutant and a branched-chain amino acid
auxotroph which is genetically engineered mutant of B. mallei using newly constructed allelic exchange vector, as vaccines in mice. The auxotrophic mutant was found to
enhance the Thl response and with a survival rate of 25% for one month post-challenge in comparison to control where none survived beyond five days (Ulrich et al., 2005). The 6-deoxy-heptan Capsular Polysaccharide (CPS)
of B. mallei, having both a pathogenic determinant and a protective antigen, is being exploited for developments of novel vaccine against glanders (Burtnick et al., 2012). Clinical and serological recovery is rare, recovered
animals are also not immune, so every animal positive for glanders should be destroyed and remaining animals should be retested at intervals of 3 weeks until all reactors have been removed:
In case of death due to glanders, carcass should
not be opened. It must be buried or incinerated
(Khan et al., 2013)
• Adequate compensation to the owners for
destroying the horses
• Manure, bedding and feed residue should be burned
or buried
• Follow vigorous disinfection programme for
premises, feed and water trough etc
• The entire suspect, in contact animals must be
isolated, properly tested and positive animal should
be destroyed
• There should be restriction of the movement of
horses
• Strict isolation, proper hygiene and sanitation
procedures should be adopted
• Disinfection of surroundings of dead or i. nfected
animals should be done as B. tnallei is highly
susceptible to common disinfectants like
benzalkonium chloride, iodine, mercuric chloride in
alcohol, potassium permanganate, 1% sodium
hypochlorite, 70% ethanol and 2% glutaraldehyde. It
is less susceptible to phenolic disinfectants. It also
destroyed by heating to 55°C for 10 min or by
ultraviolet irradiation
• Contaminated material should be cleaned with a
solution of 1 part household bleach (0.5% sodium
hypochlorite solution) to 9 parts water
• Veterinarians, animal handlers and persons i. ncontact
with infected animals should follow appropriate
biosafety measures, wear gloves and masks during
animal handling
• Awareness programmes about the glanders need to
be carried out from time to time (Khan et al., 2013)
Employing the new generation developments and
progress in vaccineess and vaccinology, safer and effective vaccines need to be focused for countering this important disease having high zoonotic potential (Paul-Pierre, 2009;
Dhama et al., 2008, 20130. Judicious application of drugs and alternative and novel/emerging therapeutic
modalities should also be kept in mind for treating
glanders (Mahima et al., 2012b; Dhama et al., 2013g, h;
Tiwari et al., 2013a, b, c). Nowadays, one health and one medicine approach is being given due importance to counter deadly pathogens, emerging/re-emerging
infectious diseases and their zoonotic threats which need to be applied from all aspects for combating glanders.
Reporting notifiable animal diseases
Many animal diseases are highly contagious and must be reported as soon as an outbreak is suspected. These are known as notifiable diseases. Once an infectious disease has been detected / suspected. It must be notified to the local health authority
A notifiable disease is any disease that is required by law to be reported to government authorities. The collation of information allows the authorities to monitor the disease, and provides early warning of possible outbreaks. • Potentially dangerous to human or animal health. Also called Reportable disease. • Occurs during pandemics. Notifiable diseases are usually operative through legal acts. • State Government do not have any specific Act , except the Epidemic Diseases Act 1897. Diseases are notifiable under International Health Regulations (IHR) to WHO in Geneva ; under the IHR. • Information is published by WHO on world wide basis.
What happens if a notifiable disease is confirmed
If a notifiable disease is confirmed:
1. Action will be taken on the infected premises to reduce the risk of the disease spreading, including movement restrictions. For some diseases, like foot and mouth disease and African swine fever, this will include culling all susceptible animals. Premises are then cleaned and disinfected with strict rules on restocking.
2. The government investigates where the disease came from and whether it has spread.
3. The government puts restrictions on all premises where the disease is likely to have spread from or to (for example when animals have been moved).
4. Further restrictions in a wider area may be introduced, depending on the risk of the disease spreading. In the case of foot and mouth disease in particular, animal movements would be restricted throughout the country. For some diseases control zones are automatically applied.
5. The following activities that could spread disease may be banned:
• hunting or shooting
• animal gatherings (like shows)
• exports
How to prevent notifiable diseases
You can help prevent notifiable diseases by following:
• strict biosecurity practices
• rules on imports and exports
• rules on feeding to farmed livestock
Animals or birds spared from culling
For most notifiable diseases, there are legal powers to cull animals to prevent the spread of disease during an outbreak.
Certain animals and birds, including breeds at risk, may be spared from culling if this doesn’t compromise controlling the disease (this isn’t guaranteed).
Compensation when animals are slaughtered compulsorily.
For some notifiable diseases, you may get compensation if your animals or birds are compulsorily culled.