HAEMOGLOBINURIA IN DAIRY ANIMALS-DIAGNOSIS, TREATMENT & PREVENTIVE MEASURES
Compiled & Edited by-DR RAJESH KUMAR SINGH ,JAMSHEDPUR,JHARKHAND, INDIA, 9431309542,rajeshsinghvet@gmail.com
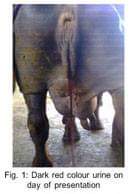
It is disease of high producing animals. It occurs after parturition and is characterized by straining during defecation, red urine, hemoglobinurea, anemia; and death may occur in this disease.Related to this, some diseses in cattle are there where the symptoms of blood are found in urine they are-
- post parturient hemoglobinuria .
- Paralytic Myoglobinuria (AZOTURIA).
- Hyperkalemic Periodic Paralysis
- Babesiosis
Here in this case we will discuss the case of post parturient hemoglobinuria which is more prominent and significant in the dairy cattle context in winter .
Etiology:
The major cause of this disease is phosphorus deficiency. It is more common in buffalo as compared to cattle.
Predisposing factors:
• The diet deficient in phosphorus leads to post parturient hemoglobin urea.
• There is deficiency of phosphorus in plants like turnips, brassica, reddish leaves and beat pulp.
• Usually animal in 3rd – 4th lactation are more prone to this disease as compared to in first, second lactations.
• Deficiency of copper in soil. Copper is essential part of an enzyme dismutase which is necessary for hemopoiesis.
• Animal in dry period have normal phosphorus. But lactating animals have deficiency of phosphorus and calcium. So more prone to it.
• It is more common 2-4 weeks after parturition. Incidence of this disease is low but mortality upto 50 %. This disease does not occur in beef cattle.
• Ingestion of cold water also leads to hemolysis.
Clinical Findings:
• Hemoglobinuria
• Lack of appetite
• Weakness develop suddenly
• Severe depression of the milk yield
• Dehydration develops quickly
• Pale mucous membrane
• Temperature 103.5 oF
• Feaces dry and firm
• Low oxygen carrying capacity of RBCs will not fulfill the requirement of oxygen; there will be increase heart rate and respiration. So there will be difficult breathing and fast heart rate.
• In later stages there is jaundice
• Pica may be present
• Course of disease is 3-5 days
• Animal becomes stagger, weak and recombinant
Haemoglobinuria is a common presenting clinical sign in dairy animals of all age
groups. Haemoglobinuria refers to presence of free hemoglobin in urine. Invariably the
cause is excessive intravascular hemolysis. However the cause of intravascular
hemolysis vary according to age and species in bovines. For rational treatment the
underlying cause has to be identified. This document focuses experience on the
diagnostic approach to be adopted for rational treatment and experience on the
treatments in vogue.
Epidemiology :
a. Occurrence :
Adult cows calved 2-4 weeks previously
High producing cows in lactations 3-6
Morbidity low, usually sporadic, may be . outbreak, case fatality 50% .
b. Risk factors:
Rape, other cruciferous plants in diet . Diets deficient in P, or copper or possibly Se.
Lush spring pasture
Very cold drinking water
Causes - Infectious disease
Babesiosis
Leptospirosis
Bacillary
haemoglobinuria
Susceptibility – Adult cattle
Buffaloes
Cattle-buffalo
Adult bovines
Occurrence–Common
Very rare
Not common
Not common - Nutritional
Phosphorus and/or
Copper deficieny
Water intoxication
Susceptibility——Adult buffaloes and cattle
Calves
Occurrence– Common
Common
- Poisoning
Copper
Plants
(Barseem, Onion, Brassica
family, Tumip, Cabbage, Beets)
Susceptibility -All ages
All ages
Occurrence–
Rare
Less common - Drugs
Intravenous infusion of
undiluted oxytetracycline
NSAIDS
Susceptibility—–Cattle
Occurrence–
Very rare
Diagnostic approach: For confirmatory diagnosis a minimum database is required which include examination of blood smear, plasma inorganic phosphorus and physical and chemical examination of urine. The susceptibility varies according to:
• Signalment: species and age
• Clinical signs: differentiate febrile and non febrile diseases. Observe for anemia
and jaundice.
• Differentiate between haemoglobinuria, hematuria and myoglobinuria. In some
cases color of urine may be helpful. Bright red color suggests hematuria. In case
of confusion microscopic examination of urine should be carried out. Brown or
brown black color is indicative of haemoglobinuria, myoglobinuria. For
differentiation of myoglobinuria chemical examination is essential. Add 10g of
ammonium sulphate to 10ml of urine and shake. Disappearance of color
suggests haemoglobinuria.
Babesiosis:
Babesiosis is blood protozoan infection often observed in cross bred cattle and
very rarely in buffaloes. Local breeds are generally resistant to this disease. Calves
below 6 months are resistant to infection. Even if calves are infected disease is mild and
0
short lived. Sudden onset of moderate to high fever (104-106 F) along with attendant
signs of anorexia, depression, loss of rumination are the early signs. Later on, pallor
mucosae and dark red to brown red or deep brown colored urine are the prominent
signs. Terminally severe jaundice is evident. Many severely affected animals die precipitously within 24 hours.
Treatment: effective drugs are available. Diminazine aceturate (Berenil) is effective, well tolerated safe drug. Sterilization with this drug may not be complete. Therapeutic dose is 3.5 mg/kg deep intra muscularly.
• Imidocarb propionate is effective @ 1mg/kg body weight subcutaneously. It also
maintains residual activity for few weeks.
Disease is generally acute and if treatment is delayed animal may succumb to anemia inspite of elimination of infection. Blood transfusion is essential in severely anemic animals.
Nutritional haemoglobinuria:
This is associated with low blood phosphorus levels. A prolonged hypophosphatemia is a major predisposing factor. Concurrent copper deficiency potentiates this disease. Buffaloes are more susceptible to this condition. Often disease appears during lactation and sometimes in late pregnancy.
Haemoglobinuria is the first sign. Urine color ranges from deep brown to black
frothy. Animal lack other systemic signs and illness goes unnoticed till anemia becomes
profound. At this stage appetite and milk production is reduced. Some animals show
signs of severe constipation and strain to defecate. Terminally recumbancy occurs and
on examination mucous membranes are pale icteric. These are bad prognostic signs.
Diagnosis can be confirmed by determining plasma inorganic phosphorus (Pi). Plasma
Pi is below 3.0 mg/dl.
Specific therapy is intravenous administration of 60g of sodium hydrogen ortho
phosphate (NaH PO .2H O) dissolved in 5% dextrose solution. Treatment is continued
at 24 hour interval unlit abnormal urine color disappears. Concomitantly oral
phosphorus supplementation in the form of dicalcium phosphate/ mineral mixture @ 60-
80g till recovery. To minimize the risk of haemoglobinuric nephrosis fluid therapy with
normal saline is advisable till recovery. These are studies which substantiate that
recovery can be enhanced by simultaneous intra venous administration of copper
glycinate (120 mg) in fluid. Intravenous administration of 40-50 ml of 10% ascorbic acid
also reduces recovery period. There are reports that ascorbic acid is effective in treating
less severe cases. Blood transfusion required in severely anemic cases @ 10-15 ml/kg
body weight.
Haemoglobinuria due to plant toxicities is generally less severe. Intravenous infusion of ascorbic acid is treatment of choice.
Bacterial causes: Leptospirosis and bacillary haemoglobinuria are the outstanding causes. Acute septicemic form of Leptospirosis characterized by causing intra vascular hemolysis, haemoglobinuria and fever. Primarily effect calves during first month of age. Clinical signs of septicemia are high fever, and petechiation of mucosa accompanied by signs of intravascular hemolysis.
Adults suffer from sub acute and chronic form. Only sub acute form may produce
intravascular hemolysis but of less severity. A consistent accompanying sign is blood
stained milk with any physical change in udder. Abortion in adult pregnant females may be another evidence of Leptospirosis. Treatment of Leptospirosis is best done by streptomycin @ 12mg/kg BID for 3-5 days. For complete sterilization single injection @ 25mg/kg is recommended.
Bacillary haemoglobinuria: very acute, toxemic and endemic disease characterized
by diarrhea, fever, abdominal pain and sudden death. Differentiation is done by blood
film examination. Feces are dark brown or there may be diarrhea with much mucous
and some blood. Differentiation from Leptospirosis clinically is impossible. Specific
therapy includes use of penicillin @ 20,000 to 30,000 units/kg or tetracycline @ 10-15
mg/kg body weight.
Paroxysmal haemoglobinuria:
It is a common condition observed in calves of 2-10 months of age. Often the sign appear few hours after drinking water.
Clinical signs may vary and in most of the cases haemoglobinuria is the only
clinical sign. Animal recover in 3-4 hours. In more severe form, nervous signs may
accompany. There is hyperesthesia, muscular tremors, nystagmus and lethargy. Very
rarely calves may develop hypothermia, edema of eyelids, arrhythmia and ruminal
tympany. Diagnosis is based on age, history of haemoglobinuria after water intake.
Treatment with hypertonic saline (5%) @ 0.5-1ml/kg i.v. may be used in mild to
moderate form of cases. In severe cases combination of 5% dextrose and hypertonic
saline achieve better response. If required tranquilizers may be used.
Diseases causing Hematuria - Pyelonephritis
- Idiopathic hematuria
- Enzootic bovine hematuria
Pyelonephritis: Refers to purulent inflammation of urinary bladder, ureters and renal pelvis. Clinical presentation varies from case to case. Passing of blood stained urine may be only early presenting sign. In other animals episodic colic along with painful frequent urination may be present. Rectal examination may reveal enlargement of ureter and kidneys with loss of lobulation (pyuria, hematuria).
Confirmation of pyuria, hematuria on urine analysis is sufficient for diagnosis.
Treatment with antibiotics viz. ampicillin, potentiated sulphonamides, penicillin for 7-10 days is effective. Penicillin in high doses (15000 u/kg) is the preferred drug.
Idiopathic hematuria: occurrence is most common in crossbred cattle and often
appears in recurrent form. There are no systemic effect except for mild reduction in milk
production and weight loss. Blood examination show mild to moderate anemia.
Treatment is difficult however response to homeopathic treatment is possible in 50 per
cent of cases.
Enzootic bovine hematuria: It is a region specific disease often occurring in hilly
areas where moist conditions persist. Likely cause is ingestion of bracken fern. It mostly
occurs in late summer when other feed is scarce or when animals are fed hay containing
bracken fern. Poisoning requires prolonged exposure (several weeks to months).
Affected cattle suffer intermittent hematuria and anemia. Affected cattle are weak, rapidly lose weight and develop pyrexia (106 F). Once animals develop clinical
diseases, poisoning is almost always fatal.
Treatment:
• Best treatment is blood transfusion upto 5 litres.
• Sodium acid phosphate Na2H2PO4 60 g/300 ml water of which is given through intravascularly or subcutaneously. Repeat after 12 hours. Route of administration depends upon the severity of disease. 100 g Na2H2PO4 orally can be given for 5 days.
• CuSO4 (acidified) 1-2 g orally for 10-15 days. It helps in hemopoiesis.
• B-complex, dextrose (if dehydration)
HOMEOPATHIC Treatment : - Ferrum phos 6x : B.I.D / 7- 10 days
- Kali chloride 200 : with or without Phosphrous : B.I.D / 1-3 days
Control:
Avoid feeding Crusiferous plants. But if have to be given then also give wheat bran (phosphorus rich diet) along
Reference-On request