Impact of Zoonotic Diseases and the Need of One Health for All
M.Hariharan1*, N.Balamurugan1, A.Varun2 and M.Nithya Quintoil2
1Field Veterinarian, Puducherry
2Assistant Professor, Rajiv Gandhi Institute of Veterinary Education and Research
*corresponding author email: harihaaranattacku@gmail.com
Introduction
World Health Organization (WHO) defines “One Health” as an integrated and unifying approach that aims to sustainably balance and optimize the health of people, animals and ecosystems. Over the past few years, the rise of zoonotic diseases has posed an immense risk to both human and animal health. Modern impacts such as changes to natural ecosystems, expansion of agricultural lands, global tourism and trade, and urbanization are the major concerns for the spread of zoonoses. WHO defines “any disease or infection naturally transmissible from animals to humans or from humans to animals” as a zoonosis. About 60% of human diseases are caused by zoonotic pathogens, which include viruses, fungi, bacteria, protozoa, and parasites. Zoonotic pathogens can be transmitted to humans through Direct contact with infected animals, or Indirect contact with wild and domestic animals, vector-borne bites by ticks and mosquitoes, waterborne, and foodborne. The most important factors for the transmission of pathogens includes improper personal hygiene, the economic crisis in the nation, lack of awareness, inadequate surveillance, and shortage of health care. This zoonotic pathogen causes increased morbidity and mortality rates in developing countries like India. In India’s scenario, the most prevalent zoonotic diseases that pose a threat to public health include Bacterial – leptospirosis, anthrax, brucellosis, tuberculosis, plague, Parasitic – toxoplasmosis, cysticercosis, echinococcosis, Viral – rabies, Japanese encephalitis, nipah, Crimean-Congo hemorrhagic fever, kyasanur forest disease, Rickettsial – scrub typhus, Protozoal – trypanosomiasis, and leishmaniasis. The current outbreak of COVID-19 is an ideal instance of a recognized emergent zoonotic disease that is still spreading globally and causing severe effects. In order to prevent zoonotic diseases proper surveillance and monitoring, risk analysis, improvement in research side, education, and awareness.
Zoonotic Importance of Livestock and Companion Animals
Livestock and companion animals has close interaction with humans as well as the environment, which plays an essential role in the lifecycle of the particular pathogen that leads to zoonoses. The production of animal products is facing considerable demand for quality protein in terms of meat and dairy problems due to growing populations, particularly in developing nations. Global urbanization is affecting the production and distribution of food, resulting in novel wildlife-domestic contact between them causing the emergence of new diseases. Intensive livestock farming, deforestation, and conversion of forests into grazing land are some of the key elements contributing to the rise of vector-borne diseases. In India, rearing livestock is a vital revenue generator for marginal and landless farmers plus providing quality protein sources like milk, egg, meat and significantly contributes to the national economy. With 193.46 million cattle, 109.85 million buffalo, 74.26 million sheep, 148.88 million goats and 9.06 million pigs, India has the highest livestock population than other countries with increasing the risk of zoonoses. Domestic animals like cattle, sheep, goats, and pigs harbor the zoonotic pathogens that can transmit diseases to humans through direct contact or animal-originating products.
Table 1. Important Zoonotic Diseases from Livestock to Human
| Disease | Etiological agent | Species | Clinical Signs in Human |
| Anthrax (Woolsorter’s disease) | Bacillus anthracis | cattle, buffalo, sheep, goat | Cutaneous infection -Pustules, dark black scab, respiratory distress |
| Bovine Tuberculosis (reverse zoonoses) | Mycobacterium bovis Mycobacterium caprae | cattle, buffalo, sheep, goat | Persistent cough, respiratory distress chronic weight loss |
| Brucellosis (Malta fever) | Brucella melitensis B. abortus, B. suis | cattle, buffalo, pig, goat | Arthritis, seminal vesiculitis, and abortion |
| Japanese Encephalitis (vector-borne) | Flavivirus | pig | Gastrointestinal pain, nervous signs -disorientation, seizures, coma, death |
| Salmonellosis | Salmonella Enteritidis S. Typhimurium | All livestock species | Acute diarrhea, vomiting, abdominal pain, dehydration |
| Cysticercosis (Taeniasis) – foodborne | Taenia solium Taenia saginata | Pig Cattle | Abdominal pain, nausea, constipation, Neurocysticercosis – epileptic seizure, headaches, blindness, hydrocephalus. |
| Q fever | Coxiella burnetii | goat, sheep, cattle | High fever (104 °F), myalgia, cholestatic jaundice, hemolytic anemia, abortion. |
The number of stray cats and dogs being adopted as pets in India is rising as people there grow more affection for their pets and more conscious of the struggles that the animals go through. The significance of proper pet ownership is highlighted in the urban region. This growing popularity for companion and exotic animals in India has resulted in an extensive range of zoonotic disease-causing organisms, placing human health care at risk. The interaction between people and their pets includes letting animals lick injuries, bite wounds, improper hygiene, sleeping with pets, allowing them into cooking area, owning exotic animals, and bringing in rescue animals, which have increased the danger of zoonotic diseases. Animals can transmit pathogens like parasites, bacteria, viral, and fungal through direct contact such as coughing, sneezing, scratching, handling pets, or by their body secretions, and indirect contact, through contaminated food, water, bedding, or by vector bite. Young children, old people, pregnant women, immune-compromised patients, veterinarians, and animal attendants are at a higher risk of zoonosis due to their contact with pets.
Table 2. Important Zoonotic Diseases from Companion Animals to Human
| Disease | Etiological agent | Species | Clinical Signs in Human |
| Toxoplasmosis | Toxoplasma gondii | cat | Abortion, stillbirth, visual disabilities in newborn child |
| Cat Scratch Disease | Bartonella henselae | cat | regional lymphadenopathy, maculopapular eruptions on bite\scratch site |
| Pasteurellosis | Pasteurella multocida | dog, cat | bite site – cellulitis, purulent exudate, osteomyelitis, endocarditis |
| Echinococcosis (Hydatid disease) | Echinococcus granulosus | dog | Growth of cysts in the liver and lungs – discomfort in the upper abdominal, and chest region, death |
| Leptospirosis (Weil’s disease) | Leptospira interrogans serovars | dog, cat | Icteric, meningitis, pulmonary hemorrhage, kidney failure, death |
| Psittacosis (parrot fever) | Chlamydia psittaci | parakeets, parrots, budgerigars, domestic birds | Shortness of breath, sore throat, pneumonia, endocarditis |
Rabies – A potential threat
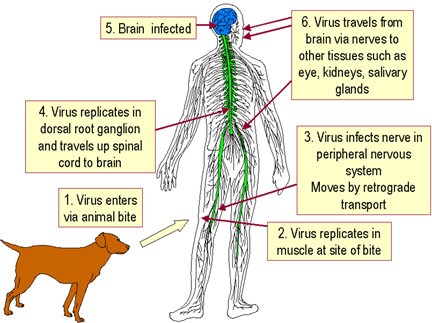
Rabies (Mad Dog disease) is a well-known fatal zoonotic disease caused by Lyssavirus family Rhabdoviridae – enveloped, bullet-shaped RNA virus. Warm-blooded animals are vulnerable to rabies virus infection, mammals act as the reservoirs for the virus. Felidae and Viverridae have high susceptibility, whereas dogs, sheep, goats, and primates with moderate susceptibility. Rabies is primarily transmitted by the bite of an infected animal with the virus in its saliva. In countries like America, Africa, and Australia rabid bats transmit the disease. Dog-mediated rabies is a major public health concern in India, with a 60,000 global death rate in which India reported more than 36% (18,000 – 20,000 deaths) of the total rabies deaths annually. Children under the age of 15 account for 30 – 60 % of recorded rabies cases and fatalities in India, as bites from animals frequently go unnoticed in this age group. The incubation period of rabies is predisposed by factors such as the Age of the victim, bite depth, and distance between the bite site and the central nervous system (CNS). The central nervous system is the site where the rabies virus enters and spreads, at a rate of up to 100 – 400mm per day, viruses propagate passively through intra-axonal flow in peripheral neurons. The development of observed clinical symptoms corresponds with viral intraneuronal dissemination, at this time the prognosis is grave.
Table 3. Two forms of rabies – Furious and Paralytic form
| Clinical Signs in Dog | Clinical Signs in Human | |
| Furious/ encephalitic form (most common) | restless and irritable, increased responses to stimuli, photophobic, pica, aggression towards the owner, striking movement, muscular tremors, weakness, incoordination. | hydrophobia, agitation, hypersalivation, seizures, hallucination, change in behavioral habits, confusion, excess salivation. |
| Paralytic/Dumb form | Lower Motor Neuron paralysis, Mandibular and laryngeal paralysis, dropped jaw. | Progressive flaccid paralysis of the bitten limb, urinary incontinence, respiratory insufficiency, coma. |
Rabies: Effective Preventive and Control Measures
- Proper disease surveillance and diagnosis – History, Clinical signs, direct fluorescent antibody (DFA) test, RT-PCR, and Serological tests.
- Post-exposure vaccination – The victim should be vaccinated immediately after the bite incident. Five doses of intramuscular injections of cell culture vaccines are administered on day 0, 3, 7, 14, 28.
- Pre-exposure vaccination – An approach to preventing rabies exposure from infected animals by immunization. People (veterinarians, zoo workers, NGO workers) who are at a high risk of coming into touch with rabid animal fluid secretions or saliva will benefit the most from this procedure. Three doses of intramuscular injection were administered on day 0, 3, 28.
- Spreading awareness and knowledge about bite wound management, and the importance of vaccination, among the people – Control measures have been undertaken however, a key barrier remains a lack of community knowledge. Despite these measures, rabies poses a severe threat to the human population.
- Implementing many rabies control policies and programs by the government – Animal Birth Control of Dogs Rules, 2001, National Rabies Control Program, 2013.
- Several non-governmental organizations (NGOs) are also involved in the fight against rabies by creating awareness among people and implementing the ABC protocol, and mass vaccination programs against rabies.
Comprehensive One-Health Approach to Rabies
Fragmented approaches to rabies control result in a lack of coordination among government, NGOs, and private sector. A “One Health approach” based on cross-departmental collaboration is more effective. Collecting the required data and sharing the data between professional sectors can help in identifying the problematic areas and helps in the development of new management strategies, and overcoming the problems in lack of coordination between the sectors. World Health organization’s One Health Initiative, is in collaboration with global alliances, and focuses on a comprehensive approach that includes improved researches on medical interventions like vaccination, wound cleaning, post-exposure prophylaxis, and rabies prevention strategies to reduce the burden of rabies in humans. WHO is working towards achieving zero human deaths from rabies by 2030. The most effective short-term option is an integrated managemental strategy that links the veterinary and public health sectors. Long-term combining the measures at the local, national, and international levels, helps in permanent control can be achieved.
Conclusion
Zoonoses cause an immense threat to both human and animal health, so they require necessary hygiene standards, and proper management in breeding, feeding, and housing. However, there is a serious disconnect between veterinary care and public health care which causes underreported case instances. In order to solve this, more time and investments are required to improve the research and development policy that helps to incorporate the betterment of disease monitoring. To promote both animal and human welfare, a “One Health” approach is required. One Health has the potential to bridge gaps between both veterinarians and healthcare personnel resulting in common preventative care. Additionally, it requires good public health infrastructure, trained primary health workers, surveillance, and quarantine measures with the ability to diagnose, treat, prevent, and manage zoonotic infections early on.