IMPORTANCE & INTERPRETATION OF LIVER FUNCTION TESTS (LFTs) IN DOGS
Liver disease can be frustrating to diagnose. Although in the dog (in contrast to the cat), it is uncommon for a patient to have normal clinical pathology values in the presence of significant liver disease, enzymology and other clinical pathology tests rarely indicate the type of liver pathology present. In addition, even liver “specific” enzymes such as ALT can be increased in non-primary hepatic disease and care must be taken in interpreting slight or even moderate increases. This lecture will focus on the tests that may be utilised in the diagnosis of liver disease and the non-hepatic causes for changes in these tests that the clinician should be aware of when interpreting clinical pathology results.
Diagnostic tests
Alanine aminotransferase (ALT, formerly SGPT). ALT is a liver specific enzyme in the dog and cat. The highest cellular concentrations occur in the cytosol therefore the enzyme is released following severe, acute and diffuse hepatocellular necrosis. In general, serum levels are not regarded as significant unless they are two to three times above normal. Mild-moderate increases in ALT (up to four to five times normal) may occur with non-hepatic disorders such as inflammatory GI disease, cardiac failure and haemolytic anaemia.
The serum half-life of ALT is less than 24 hours. Levels peak two to three days after hepatic insult and return to normal in one to three weeks if hepatic insult resolves. A persistent increase indicates continuing hepatocellular insult. ALT levels may also be moderately increased in animals on anticonvulsant therapy and glucocorticoids and with biliary stasis.
Alkaline phosphatase (ALP). ALP is bound to membranes of bile canaliculi and bile ducts. Values are increased by any condition causing cholestasis, either intra- or extra-hepatic. Cholestasis results in increased synthesis and regurgitation of the enzyme from the biliary system into the serum.
Isoenzymes. Other isoenzymes of ALP are also found in bone, intestine, kidney tubules and the placenta. However, the half-life of the intestinal, renal and placental isoenzymes are so short (two to six minutes) that serum elevations of ALP would rarely occur from these organs. Usually an elevation in ALP is due to hepatic or bone isoenzymes. However, exogenous and endogenous glucocorticoids can induce a specific isoenzyme and thus result in elevated serum levels in the dog (but not in the cat). The value in measuring the ALP isoenzyme in the diagnosis of hyperadrenocorticism is highly questionable as the isoenzyme is increased by hepatic pathology as well as hyperadrenocorticism.
ALP levels will be increased in young growing animals (bone isoenzyme) and in destructive bone disease. ALP is also increased in certain carcinomas and mammary gland tumours, and with anticonvulsant therapy in dogs, but not cats.
ALT vs. ALP—does their relative increases help determine the location of liver pathology (intra- or extra-hepatic)?
Serum enzymology is not particularly helpful in determining whether an animal has hepatic or post-hepatic disease. Post-hepatic obstruction of the biliary tract almost invariably causes secondary hepatocellular damage and hence both ALT and ALP will be elevated. ALP is elevated by both intra- and extra-hepatic cholestasis thus is increased in hepatic and post-hepatic disease.
The relative degree of increase of each enzyme is also not helpful; in fact, if ALP is substantially increased and ALT normal or only slightly increased, non-hepatic disease such as hyperadrenocorticism or exogenous corticosteroid administration is more likely to be present.
It is important to be aware that serum enzymes are not liver function tests and there is no correlation between the magnitude of the enzyme increase and the severity or reversibility of the condition. Occasionally, cases of severe liver dysfunction, e.g., biliary cirrhosis, neoplasia or portacaval shunt, may be associated with minimal or no increases in serum enzymes.
Gamma glutamyl transpeptidase (GGT). GGT levels are increased in most conditions that cause elevation in ALP, i.e., cholestasis, glucocorticoid therapy, hyperadrenocorticism. However, unlike ALP, GGT is not elevated with increased osteoblastic activity (e.g., growing dogs) and may not be elevated in dogs on anticonvulsant medication. ALP is slightly more sensitive than GGT for detection of cholestatic disease in dogs
Serum protein
Serum albumin. Albumin is synthesised only in the liver. A loss of greater than 70% of liver function is required before hypoalbuminaemia occurs. Hypoalbuminaemia most commonly occurs in cirrhosis and portosystemic encephalopathy but will also occur in severe diffuse necrosis. Albumin concentrations may also be decreased in renal and gut disease, severe cutaneous burns, protein malnutrition, in the presence of acute phase reactants, and in patients with exudative effusions (which cause sequestration of albumin).
Serum globulins. Increased serum globulin levels may occur in inflammatory hepatic disease or when the hepatic reticuloendothelial system is compromised. Decreased levels will often occur in portosystemic encephalopathy as a large proportion of globulins are synthesised in the liver.
Bilirubinaemia and bilirubinuria
Dogs (males more than females) have a low resorptive threshold for bilirubin. They also have renal enzyme systems that produce and conjugate bilirubin to a limited extent. Therefore, mild bilirubinuria (up to 2+) can occur in normal dog urine of greater than 1.025 specific gravity.
Slight bilirubinuria may occur in starvation and febrile states and mild bilirubinaemia and bilirubinuria can also occurs with sepsis. Bilirubinuria will develop well before overt jaundice in dogs due to the low renal threshold.
Is the relative ratio of conjugated vs. unconjugated bilirubinaemia helpful in determining whether hepatic pathology is intra- or extra-hepatic?
While an animal with only conjugated bilirubinaemia would most likely have post-hepatic jaundice (due to biliary tract or pancreatic disease most commonly), the majority of animals with hepatic or post-hepatic jaundice will have both unconjugated and conjugated bilirubinaemia. Post-hepatic obstruction will cause secondary hepatocellular damage and, as previously mentioned, bilirubin excretion is the first process to become disordered in primary hepatocellular disease.
Cholesterol
Very low serum cholesterol concentrations may occur in patients with congenital or acquired portosystemic shunts and fulminant hepatic failure. Increased serum cholesterol in a jaundiced patient usually indicates major bile duct occlusion particularly in cats. However, cholesterol concentrations are also increased in non-hepatic diseases such as pancreatitis, diabetes mellitus, hyperadrenocorticism and hypothyroidism which if present concurrently can confuse interpretation.
Bile acids
Serum bile acids are a sensitive and specific measure of hepatobiliary function in the cat and dog. They should be considered when other routine clinical pathology results do not permit an unequivocal diagnosis of liver disease to be made. It is not necessary to do the test if the patient is jaundiced and not anaemic, nor if liver enzyme changes permit an unequivocal diagnosis of liver disease to be made.
Bile acids are useful as a screening test for hepatic encephalopathy (except in Maltese Terriers). Their major advantage in this context is the lack of stringent requirements for sample collection and processing in contrast to blood ammonia determination.
Occasionally, bile acids can be normal in patients with hepatic disease. We have observed this in some cases of hepatic neoplasia. The level of serum bile acid increase roughly correlates with the severity of the hepatobiliary disorder but the level gives no indication of reversibility or the type of the lesion and hence prognosis.
Serum bile acid concentrations are usually not affected by steroid administration but occasionally can be markedly altered due to alteration of hepatic architecture as a result of hepatic glycogen accumulation. Serum bile acids are therefore useful but not infallible for differentiating elevated ALP values due to steroids (endogenous or exogenous) or hepatobiliary disease.
Other diagnostic procedures
Radiology
Plain radiographs may be helpful in confirming hepatomegaly, the presence of a small liver, or asymmetric enlargement of a liver lobe. However, although the liver is the largest solid organ in the body, its plain film evaluation is unreliable. Contrast radiography is primarily indicated in diagnosing portacaval shunts.
Ultrasound
Ultrasound examination of the liver may assist in differentiating homogeneous enlargement from cellular infiltration and in differentiating hepatic from post-hepatic cholestasis.
Biopsy
Hepatic biopsy is usually the only method by which the type of hepatic pathology can be characterised. Hepatic biopsy (via exploratory laparotomy or ultrasound guided) should be considered in all dogs with obstructive jaundice and in those with evidence of chronic hepatocellular disease.
The pretenders
A number of diseases may be confused with hepatic disease because of clinical signs or clinicopathological abnormalities. Increased liver enzymes, ALT, and ALP may occur in pancreatitis, diabetes mellitus, and hyperthyroidism. Moderately increased bilirubin can occur in a variety of non-hepatic diseases as well as in conditions such as prolonged anorexia, catabolic states, and infection. Mild increases in ALT may be observed in animals with cardiac pathology. Substantial increases in ALP with moderate increases in ALT will occur in most dogs with hyperadrenocorticism.
Causes of hepatic disease in dogs
Chronic hepatitis
Chronic progressive hepatitis-idiopathic, immune mediated?
Bedlington Terriers, WHW Terriers—copper toxicity
Lobular dissecting hepatitis
Leptospirosis
Viral—adenovirus
Drug induced- primidone, phenytoin
Suppurative cholangiohepatitis
Non-suppurative (lymphocytic) cholangiohepatitis
Acute hepatitis
Toxins e.g., thiacetarsamide, anticonvulsants
Aflatoxin, bacterial endotoxin, blue green algae
Bacterial- Leptospira, Salmonella, Clostridia
Viral- adenovirus I (ICH), canine herpes
Toxoplasmosis
Dirofilariasis—caval syndrome
Acute pancreatitis
Acute haemolytic anaemia
Heat stroke
Surgical hypotension or hypoxia
Trauma
Cirrhosis
End-stage fibrosis of many inflammatory hepatic diseases. Aetiology undetermined in majority of cases.
Glucocorticoid hepatopathy
The canine liver is uniquely sensitive to the effects of exogenous or endogenous corticosteroids.
Neoplasia
The liver is a frequent site for both primary and metastatic neoplasia.
Primary neoplasms
Hepatocellular carcinoma
Hepatoma
Cholangiocarcinoma
Fibroma/fibrosarcoma
Haemangioma/haemangiosarcoma
Lymphosarcoma (may also be multi-focal)
Portosystemic or hepatic encephalopathy
The liver is a crucial organ in the human body, and is responsible for handling various metabolic functions in the body. One of the most important roles of the liver is to detoxify the blood by processing different waste products in the hemoglobin. To conduct all of these functions properly, the liver produces and secretes several types of enzymes for optimal regulation. SGOT (Serum glutamic oxaloacetic transaminase) and SGPT (Serum glutamate pyruvate transaminase) are two of the most common enzymes produced by the liver. SGPT test, or Serum Glutamic Pyruvic Transaminase, is a blood test that can be used to detect any liver problems. It is commonly used to measure the level of a specific enzyme called ALT (alanine aminotransferase), a specific enzyme that is released when the liver is damaged or inflamed. If a patient has a high level of ALT, it may indicate that his liver has been damaged. However, if the results are at the SGOT test normal range then it is usually a sign that his liver is functioning properly.
What The Liver Does
The liver is one of the largest and most important organs in your dog’s body, performing about 500 daily tasks (in combination with other organs). Here are just a few of the liver’s key activities:
Detox
First, the liver clears potentially toxic chemicals from both inside and outside the body, including drugs, vaccines, environmental toxins and even intestinal microbes. In order to detox, the liver needs critical antioxidant nutrients and enzymes such as glutathione (an important antioxidant molecule that helps prevent aging and chronic disease). The liver detoxifies harmful substances by a complex series of chemical reactions. The role of these various enzyme activities in the liver is to convert fat-soluble toxins to water-soluble substances. Once these substances are bio-transformed and no longer toxic, they then exit the body via urine or bile.
Storage
The liver is a storage unit, storing sugar as glycogen and regulating blood sugar levels. The liver also stores nutrients like iron, copper, vitamins B-12, A, D, E and K.
Production And Regulation
The liver is all about production, including:
- Production of bile, which aids the digestion of fats.
- Production of blood proteins, clotting factors and substances important to the making of red blood cells. Red blood cells, which carry oxygen around the body, are also recycled in the liver.
The liver also regulates a number of hormones and neutralizes free radicals produced during oxidation with antioxidants like vitamins C and E, as well as glutathione.
Nutrient Breakdown and Absorption
The liver not only breaks down nutrients from the diet, it also helps the body use those nutrients in the buildup of tissues. There is hardly a more important organ in the body and so when the AST, ALT, ALP and GGT all start to elevate, what does this mean?
High Liver Enzymes In Dogs
There are other liver measurements you’ll see in your dog’s blood panel, but I want to focus on the liver enzymes and what they mean.
- AST – Aspartate transaminase (formerly SGOT or serum glutamic oxaloacetic transaminase). If your dog’s AST is elevated, it may come from the liver but this enzyme is also found in red blood cells, heart, muscle, pancreas and bile. So if your dog’s AST isn’t normal, your vet should find out what’s causing the elevation. AST is normally low in serum so should be measured along with ALT as part of a liver panel to see what’s going on.
- ALT – Alanine aminotransferase (previously called SGPT or serum glutamic pyruvic transaminase). If it’s elevated, ALT can signify liver or hepatic alert as to liver cell death … but this enzyme also comes from the kidney as well as the intestines, so liver problems aren’t necessarily the only cause of elevated ALT, and further analysis is warranted.
- ALP – Alkaline phosphatase is found in bone, kidney, bowel (intestines) and the placenta (if pregnant), as well as the liver. The levels of this enzyme are highest in the bone and the liver. Basic phosphatase is a homodimeric enzyme that is high in young fast growing animals, so it’s not unusual to see elevated ALP in young dogs. But whatever your dog’s age, if ALP is elevated, ask your vet to investigate the reason.
- GGT – Gamma glutamyl transferase. This enzyme is useful for diagnosing and monitoring hepatobiliary (liver and bile) disease. GGT is the most sensitive enzymatic indicator of liver disease. If you’re concerned about your dog’s liver health make sure that your veterinarian includes GGT as a part of the panel.
I really want to emphasize the need for a GGT test. Not all veterinarians measure this enzyme but it’s a really important one, so make sure you ask for it.
What is SGPT and SGOT?
SGPT and SGOT are two of the most common types of liver enzymes. When liver cells are damaged or inflamed, these enzymes can leak into the bloodstream, causing elevated levels of SGOT and SGPT in a blood test. As a result, these enzymes are commonly used as markers of liver function and can help diagnose liver diseases such as hepatitis, cirrhosis, or liver cancer. Besides the liver, SGOT is found in the kidney, muscles, heart and even the brain. On the contrary, SGPT is predominantly found in the liver only. Elevated levels of either of the enzymes can result from:
- SGOT levels can rise during liver complications, heart attacks or muscle injuries.
- SGPT levels can rise during liver diseases and damage to the tissues in the liver.
However, elevated levels of SGOT and SGPT can also be caused by other factors such as alcohol consumption, certain medications, or muscle damage. The SGPT levels are more inclined towards determining liver diseases and damage due to its elevated levels.
What are the symptoms of elevated SGPT and SGOT levels?
If you see a doctor with the following symptoms, they might suggest undergoing the SGPT & SGOT tests. However, in most cases, elevated SGOT and SGPT levels may not cause any noticeable symptoms. Some people may experience mild symptoms such as –
- Constant feelings of fatigue and tiredness
- Vomiting and nausea
- Abdominal discomfort
- Bruising quickly
In more severe cases, liver disease can cause symptoms such as –
- Jaundice
- Shortness of breath
- Swelling in the leg
- Swelling in abdomen
- Dark urine
- Pale stools
Experiencing these symptoms is a warning sign that you need immediate medical intervention. If the test reports come back with high SGOT and SGPT levels, your doctor will move ahead with further testing or proceed with the treatment.
How is the SGPT/SGOT Blood test is Performed?
The SGPT test is performed by obtaining a blood sample from a vein in the arm. This sample is then analyzed by a qualified technician at a laboratory. A test report is then generated, which will provide the results in units per liter of blood. The test results are useful in detecting liver diseases and in diagnosing hepatitis. It is also used in monitoring the effects of medicines that may damage the liver. It is a painless procedure and does not require special preparation. Typically, the test can be performed within five minutes. Your doctor will prescribe getting an SGPT & SGOT test to analyze your liver function and rule out possible complications.
What are normal levels of AST (SGOT) and ALT (SGPT)?
The SGPT and SGOT test normal range are standard. However, the range can slightly vary, depending on the testing method in the laboratory.
- Normal SGOT levels– 5 to 40 units per liter of serum
- Normal SGPT levels– 7 to 56 units per liter of serum
If the blood test reports are drastically different than the normal range, it can signify potent complications in the body, especially with liver diseases and disorders.
What do Elevated SGPT and SGOT levels Indicate?
Since SGPT and SGOT are quintessential enzymes produced in the liver, it isn’t surprising that altered levels of these enzymes indicate signs of liver damage. The high levels are often indicative of several underlying complications in the body such as viral hepatitis, alcoholic liver disease, non-alcoholic fatty liver disease, cirrhosis, or liver cancer. However, elevated SGPT and SGOT levels can also be caused by other factors such as certain medications, strenuous exercise, or muscle damage. Therefore, it is important to consult with a healthcare provider to determine the underlying cause of elevated SGPT and SGOT levels. Regular monitoring of liver enzymes can also help to detect liver disease early and prevent long-term liver damage.
Are SGPT and SGOT Indicative of Liver Disease only?
As we mentioned, that isn’t the case at all. Lower or elevated SGPT and SGOT enzymes aren’t just tied with liver disease or liver function. Sometimes, patients with elevated levels of these two enzymes have optimal liver function.
How can I prepare for the SGPT/SGOT Blood test?
The SGPT/SGOT blood tests are a part of the liver function test and are routine blood test that doesn’t require excessive prepping. The patients don’t have to fast or worry about the day when the blood is drawn. However, for accurate results, we’d recommend discussing the medications you take. Since medications can alter the final reports, your doctor might advise getting the blood drawn before taking the medications. The phlebotomist will collect the blood sample from the veins in your forearm after disinfecting the area. The collected sample is then sent for further testing to the laboratories.
Are there any risks associated with the SGPT/SGOT blood tests?
The SGPT/SGOT assessment in the body is done using a blood test. This means that the risks associated with these routine blood tests are very low and sometimes non-existent. However, in very rare cases, some of the common risks might include:
- Excessive bleeding at the puncture site
- Hematoma or clotted blood underneath the skin
- Feeling lightheaded
- Infection
What do the Abnormal Test results Indicate?
Abnormal SGPT-SGOT levels in the bloodstream can be indicative of several complications, including:
- Hepatitis
- Liver cirrhosis
- Liver tissue damage
- Liver cancer
- Tumor in the liver
- Obstructed blood flow to the liver
- Hemochromatosis or iron build-up in the bloodstream
- Mononucleosis caused by Epstein-Barr virus
- Pancreatitis
If you have lower SGPT-SGOT levels in the bloodstream, that indicates a healthy liver. Unlike other markers, a low level, in this case, doesn’t signify anything alarming.
What is the Alarming Level of SGOT and SGPT?
The normal levels of SGPT usually must lie between 7-56 units/liter of serum. However, if the level of SGPT shows more than 56 units/ liter in the patient’s blood test, then that is referred to as an alarming level. The normal level of SGOT usually must lie between 8-45 units/ liter of the serum. However, anything above 50 units/liter for men and above 45 units/ liter for women can be considered as alarming. The high levels of SGOT and SGPT often indicate severe underlying complications for the patients.
Why GGT Is Important
GGT can help confirm or rule out liver problems, as well as other diseases.
Liver And Bile (Hepatobiliary) Disease
- GGT is the key liver enzyme linking lab reports to liver disease. This enzyme increases in post-hepatic biliary obstruction and can reach 5 to 30 times normal.
- If ALP is elevated but not GGT then skeletal disease is more likely the problem, and not hepatobiliary disease.
- Increased GGT and increased ALP often indicates hepatobiliary disease … but in rare cases there can be gammopathies (abnormal gamma gobulin levels) present that could lead to unreliable GGT results.
- In diagnosing infectious hepatitis, GGT is less useful than the transaminase enzymes, as it rises only modestly (2 to 5 times normal).
Other Liver Problems
- GGT is highly effective in detecting jaundice, cholangitis and cholecystitis. The rise of GGT happens earlier than other measurements and it stays high longer.
Cancer
- Huge elevations of GGT are also seen in the serum of both primary and secondary neoplasms (cancers) so it’s essential to know if those levels are high. A 2012 British study explains that GGT is a marker of oxidative stress, and high GGT levels may therefore indicate higher cancer risk (1). The same study found that curcumin, known for its anticancer effects, may help lower GGT.
Environmental Toxins
- GGT is elevated with exposure to chemicals and persistent organic pollutants (POPs) so it’s a sensitive marker for environmental toxicity.
- Elevated GGT can also indicate exposure to fungus and molds. These may be environmental or in your dog’s kibble, where mold found in corn and other grains comes in the form of dangerous mycotoxins in the food. These mycotoxins can cause liver failure and can precede cancer of the liver so it’s important to know if your dog’s been exposed.
GGT Can Help Rule Out Other Diseases
- Patients with renal failure and skeletal or muscular diseases can actually have normal GGT levels so GGT testing can also help exclude those diagnoses.
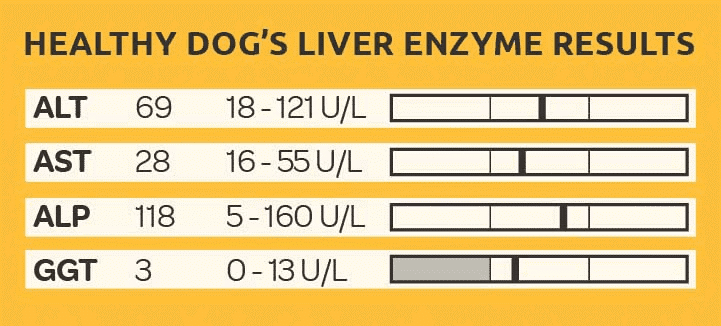
Here’s an example of a healthy dog’s liver enzyme results, showing all enzymes including GGT well within normal ranges.
Keep in mind some of the things that might cause elevated liver enzymes in dogs.
What Causes Elevated Liver Enzymes In Dogs?
The best way to preserve your dog’s liver health is to manage some of the many outside influences that can impact your dog’s liver enzyme levels. So here’s some information about what toxins cause elevated liver enzymes in dogs …
Medications
Drugs like phenytoin and phenobarbital prescribed for seizures, as well as any other drug, including heartworm medication and anti-inflammatory drugs, can result in abnormal liver enzymes, so if your dog is on any medication your vet should always consider whether that may be the cause.
Vaccine Adjuvants
Viral infections can affect liver enzyme tests and so can the vaccines for viral diseases. In humans, the Hepatitis B vaccine induces liver damage primarily when it contains the toxic vaccine adjuvant aluminum hydroxide, the common aluminum salt adjuvant in vaccines – and found in all veterinary vaccines. The aluminum hydroxide adjuvant also triggers the motor neuron autoimmunity issues seen in Gulf War Syndrome sufferers (2). This syndrome has been found to be indistinguishable from the autoimmune disease ALS or Amyotrophic Lateral Sclerosis (Lou Gehrig’s disease). This is essentially what happens in MS or multiple sclerosis, another neurodegenerative disease, and I have seen cases of this type of disease in dogs following vaccination.
Aluminum hydroxide also caused a loss of mitochondria and cell death in mouse livers exposed to low doses of the Hepatitis B vaccine. 144 genes in the mouse livers were altered in their expression only a day following vaccination. In 2002, Hepatogastroenterology reported that the Hepatitis B vaccine was associated with high risk for hepatitis, gastrointestinal disease and other liver function tests .
Endocrine Disrupting Chemicals
Other important things that can affect the liver are the EDCs or endocrine disrupting chemicals so pervasive in the environment. Hormones, pesticides and herbicides are also rampant in our water and food supply.
Can Dog Food Cause Elevated Liver Enzymes?
Yes, dog food can affect your dog’s liver health. First, as I mentioned earlier, kibble can contain dangerous mycotoxins called aflatoxins. Aflatoxins mainly affect the liver, causing jaundice, weight loss and lethargy … and the effects can be life-threatening.
Second, most processed pet foods contain synthetic vitamins and minerals, as well as pesticides and other toxins. The body has to work harder to detox these chemicals and this stresses the liver.
Third, because of the high heat of processing, kibbles also contain toxic byproducts like heterocyclic amines and acrylamides. These also create additional burden on your dog’s liver.
What To Feed A Dog With High Liver Enzymes
It’s best to feed your dog a diet that supports his liver, preferably a fresh, whole food, raw-meat based diet without any synthetic chemicals added. Feeding liver also supports your dog’s own organ … and you can add liver-supportive foods like dandelion greens, broccoli sprouts, spinach and fermented vegetables and mushrooms.
How to Treat Elevated Liver Enzymes In Dogs
In addition to feeding a fresh, whole food diet as described above, you can add some supplements that’ll support your dog’s liver.
Glutathione
Glutathione is a potent antioxidant in the body, and it helps the liver detoxify. The amino acids N-acetyl-cysteine (NAC) and S-adenosyl-L-methionine (SAMe) are glutathione precursors, so NAC and SAMe are two supplements that help the liver.
Milk Thistle
Milk Thistle, or silymarin, helps protect the liver and supports regeneration of liver cells. Buy organic milk thistle in powder or tincture form, available at most health food stores, and sometimes combined with other liver-supportive herbs. Give 1-2 drops of milk thistle tincture or 100mg milk thistle powder per 10 lbs of body weight, 1-4 times daily. If using a combination herbal remedy, follow the directions on the package.
Caution: Don’t use milk thistle in pregnant or lactating dogs and ask your vet about it if your dog’s on any medications. Many experts recommend only giving milk thistle for periods when the liver is stressed, not as a daily supplement.
How Long Can A Dog Live With High Liver Enzymes?
How long your dog can live with high liver enzymes depends on the reason for the elevated results. That’s why you need to ask your vet to include a GGT test which will help you get to the bottom of the cause of your dog’s high enzyme numbers. Once you know what’s wrong, then you can deal with the underlying problem.
The liver is the most important internal organ and is open 24/7/365. It’s involved in every bodily process so protecting liver health is essential. Following a natural lifestyle can help your dog avoid compromise to this vital organ that helps detoxify the body from our increasingly toxic world.
Compiled & Shared by- Team, LITD (Livestock Institute of Training & Development)
Image-Courtesy-Google
Reference-On Request.