Leptospirosis-An Overview
Navya Sri Bairi1* and B. Srinu1
1Department of Veterinary Public Health and Epidemiology, College of Veterinary science, Mamnoor, Warangal.
_______________________________________________________________________________________________________________________________________________________________________
*Corresponding Email: navyasribairi12@gmail.com
1Department of Veterinary Public Health and Epidemiology, College of Veterinary science, Mamnoor, Warangal.
Leptospirosis is a bacterial disease of zoonotic importance, prevalent globally and it affects most of the mammalian species including both domestic animals and wild animals. According to WHO, in India, huge and diversified animal population with their close contact with farming community is playing an important role in the spread of the disease. Leptospirosis was described as the occupational disease in the ancient China. It occurs throughout the year with high incidence during the rainy season due to the survival of leptospira in water logged conditions and slightly alkaline environment for long time. Bovine leptospirosis has been associated with serious financial loss due to infertility, abortions, high culling rates, mastitis or decrease in milk yield. The abortions of leptospirosis are due to interference with the implantation of embryo or with other pregnancy events.
Leptospira are thin spiral organisms of 0.1mm x 6 – 20mm, with tightly set coils. These are Gram negative, strict aerobes, motile by endoflagella on its long axis – by rotating (“spinning”) and bending – flexuous type of motility. Usually, one or both ends of this single-cell organism are bent or hooked. These are poorly stained by conventional methods but different staining techniques dark field microscopy, phase contrast microscopy, silver impregnation technique and immunological staining are used.
Earlier they were classified based on serological reactions into 2 species as: L. interrogans which is pathogenic and L. biflexa which is saprophytic. Currently 20 recognized species which can be classified into 3 groups viz., pathogens, nonpathogens and organisms of uncertain pathogenicity. About>250 pathogenic serovars in 24 serogroups are defined.
Synonyms: Canicola fever, Hemorrhagic jaundice, Mud fever, Swamp fever, Swine herd’s disease, Weil’s disease.
Host: Man, buffalo, camel, cat, cattle, dog, horse, pig, rodents
Pathogenesis:Organisms localize in PCT of kidneys & are excreted in urine for long by reservoir hosts without clinical signs. Many serovars of leptospirae can be roughly categorized as host adapted or non adapted.
Host adapted serovars: mild and sporadic infection, with venereal transmission and lifelong colonization of the genitourinary tract. Serovars hardjo in cattle and bratislava and tarassovi in swine are examples.
Non adapted strains: more likely to produce catastrophic infections, with abortion storms in pregnant animals and, not infrequently, death of adult hosts. The carrier state is generally brief. Serovar pomona is non adapted for swine and cattle, canicola for dogs, Icterohaemorrhagiae adapted to rats and Ballum are adapted to mice. The relationship between hosts and adapted strains gives rise to a minor but long-lasting serologic response, whereas non adapted strains provoke high antibody titres.
Leptospiral endotoxin is of low potency, compared with that of many other gram-negative bacteria. It mediates adherence of neutrophils to endothelial cells and platelets, suggesting a role in development of thrombocytopenia. LPS is immunogenic, activates HIR via TLR 2 & is responsible for serovar specificity. In acute leptospirosis, damage to vascular endothelium is common, with resulting haemorrhage and disseminated intravascular coagulation (DIC). The DIC may be mediated, at least in part, by endotoxin, but sphingomyelinase haemolysin produced by many serovars may be responsible for this vascular damage and for specific clinical signs such as haemoglobinuria.
Modes of Transmission
Carriers are major means of host-to-host transmission. By direct or indirect contact through nasal, oral, or eye mucosal membranes or abraded or traumatized skin with urine or carcasses of infected animals. Urine: Indirect exposure through water, soil, or foods contaminated by urine from infected animals is the most common route. After a short period of circulating high levels of the spirochete in their blood, animals shed the spirochete in their urine, contaminating the environment. Indirect exposure depends on environmental moisture, neutral soil pH, and a sufficiently mild climate to favour survival of leptospira. Inhalation of droplet aerosols of contaminated fluids can occasionally occur. Urine aerosols in milking parlours (especially those of the herringbone configuration). The organism can also be isolated from milk of infected cows, and this probably serves as a means of transmission to humans and calves.
|
Transmission cycle
Incubation period
The incubation period is usually 2-26 days, but usually (7 – 12 days) days
Period of Communicability or Infectious Period
Humans with leptospirosis usually excrete the organism in the urine for 4-6 weeks and occasionally for as long as 18 weeks.
Person-to-person transmission is considered extremely rare. Cases are seen sporadically throughout the year. But an outbreak occurs during the rainy season because of widespread contamination by infected rodent urine in flood water. Rodents are displaced from their burrows and drains by the water. High humidity and heavy rainfall intensify the outbreak. Rats and bandicoots distribute more virulent leptospires through their urine into the environment than other animals.
Clinical Signs:
Man: High fever, jaundice, conjunctivitis, epistaxis, death due to acute renal failure.
Animals: Periodic ophthalmia (horses), icterus, hypogalactia, still birth, abortions.
Laboratory diagnosis of Leptospirosis
Direct Diagnosis include, demonstration of the organism in body fluids by DFM, Culture and isolation of the bacteria from blood, urine or tissues, direct staining of the organisms, Immuno fluorescence, polymerase chain reaction, animal Inoculation studies etc., where as in Indirect Diagnosis, in which demonstration of antibodies to leptospires by various serological primary, secondary and tertiary immune assays or tests, namely, Microscopic agglutination test (MAT), ELISA, Macroscopic slide agglutination test (SAT), Lateral Flow assays, Indirect Haemagglutination test (IHA), Counter immuno electrophoresis (CIE), Complement –fixation test (CFT), Latex agglutination tests (LA), Indirect fluorescent antibody test (IFAT), etc., however, ELISA and MAT are the commonly used sero-diagnostic techniques.
Clinical signs with history – exposure to contamination of urine
Demonstration of Leptospires or their products: Dark field Microscopy
- Microscopy : silver impregnation method
- Dark-field Microscopy
- Phase contrast microscopy
- FAT
- Body fluids or impression smears
Fontana’s silver staining
It is used to stain the Leptospira.In this fixative solution and mordrant are used.
Culture media
Fletcher’s medium – semisolid medium, Stuart’s medium, Korthoff medium and EMJH (Ellinghauson, McCullough, Johnson and Harris) medium are used. EMJH is liquid medium supplemented with 5-10% rabbit serum or BSA & Tween 80 (long chain FAs). Since the organisms are fastidious. Contaminated samples (or cultures) can be filtered through a 0.45 µm bacteriological filter and inoculated into a medium containing 5-fluorouracil at 200 µg/mL. The media can be inoculated with one to three drops of urine within a few minutes of collection, or urine diluted 1: 10 with 1% BSA, as soon as possible after collection. 10% tissue suspension in 1% BSA (one to two drops) or a few drops of oxalated or heparinized blood. Cultures are incubated at 30°C for up to 13 weeks. A drop of the culture is examined by dark-field microscopy once weekly. Serovar Hardjo is one of the slowest growing serovars.
 |
|
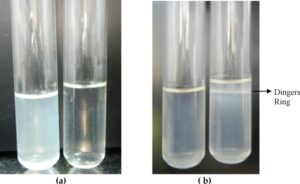
Serodiagnosis
Ideal method for diagnosis of leptospirosis is the demonstration of significant levels of antibodies to leptospires in the serum of recovered animals. Plate agglutination test with killed antigens (Macroscopic) and microscopic agglutination test (MAT) with live organisms are used as antigens. Antibodies in the test serum react with antigens on the surface of the bacteria and agglutinate them. The endpoint (titer) is taken as that dilution which gives 50% agglutination, leaving 50% of the cells free when compared with a control suspension of Leptospira is considered positive at 1:100 dilutions.
ELISAs: Detection of antibodies to the predominant serovars. Tests for the detection of both IgM and IgG are available. Use broadly reacting antigen. Serogroup cannot be identified. Readymade reagents with long shelf life. Need ELISA reader and washer.
Molecular methods are used for identification & subtyping
- PCR (serum & urine) – 16S or 23S rRNA genes of repetitive elements
- REA, RFLP, PFGE, dot blotting, in situ hybridization.
Treatment: Penicillin and Tetracyclines are generally used to treat the disease.
Prevention and Control: Prevention of environmental contamination by animal excreta. Rodent control in human habitation and agriculture fields. Provision of protective clothing to occupational workers. Do not enter pigsties or cowsheds in bare feet. Cover blisters, cuts, scratches with waterproof plasters during the work. Proper washing of the hands after handling an infected animal. Mechanization of agriculture. Avoid swimming in contaminated water. Disinfection of swimming pool with chlorine, kennel with cresol and agriculture field with copper sulphate. Regular immunization of animals. 7 in 1 vaccine is available for dogs which contains in activated Leptospira Canicola and icterohaemorrhagica. Infected bulls should not be used for breeding purpose. Maintenance of hygienic conditions in sheds and kennels.



