One World, One Health Prevent Zoonoses: Stop The Spread
Dr Rooh Ul Amin
Veterinary Assistant Surgeon
Department of Animal Husbandry Kashmir
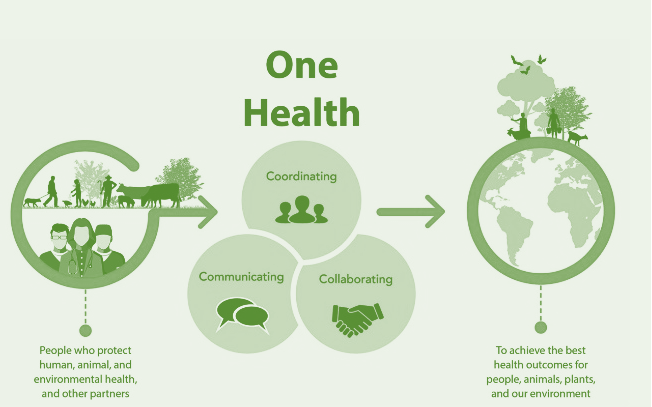
The concept of “One World, One Health,” is based on the understanding that humans, animals, and the environment are inextricably linked, indicating that the world has suddenly realized the interrelation between ecology, animal diseases, and public health, striving to restore and maintain harmony and synergy. One Health approach has assumed an extraordinary level of importance over the past decade while taking into account the boundaries between human, animal, and environmental health. The One Health approach is a practical model that aims to prevent and address zoonotic diseases by integrating human, animal, and environmental health. By linking humans, animals and the environment, One Health can help to address the full spectrum of disease control – from prevention to detection, preparedness, response and management – and contribute to global health security. Human populations are growing and expanding into new geographic areas. As a result, more people live in close contact with wild and domestic animals, both livestock and pets. Animals play an important role in our lives, whether for food, fiber, livelihoods, travel, sport, education, or companionship. Close contact with animals and their environments provides more opportunities for diseases to pass between animals and people. The environment plays an important role in one health concept and acts as a bridge between human and animal health and influencing the occurrence and spread of diseases [1,2]. The earth has experienced changes in climate and land use, such as deforestation and intensive farming practices. Disruptions in environmental conditions and habitats can provide new opportunities for diseases to pass to animals. The World Health Organization (WHO) estimates that one in every four deaths globally can be attributed to environmental factors. As per OIE 60% of known human infectious diseases have their source in animals (whether domestic or wild), as do 75% of emerging human diseases and 80% of the pathogens that could potentially be used in bioterrorism. Some estimates suggest that world production of food animals is reduced by more than 20% due to disease, which means that even animal diseases not transmissible to humans may lead to serious public health problems due to the shortages and deficiencies that can follow. The earth has experienced changes in climate and land use, such as deforestation and intensive farming practices. Disruptions in environmental conditions and habitats can provide new opportunities for diseases to pass to animals. Hence, our collective responsibility is to prevent, predict, detect and respond to global health threats. Our current understanding of the various interactions between humans, animals, plants and the environment must be re-evaluated.
There is sufficient evidence supporting the notion that no single department or sector can effectively address the current challenges that affect One Health (3). One Health was developed to recognise that the health of humans, animals, plants and the ecosystem is interrelated (4). The foundation of this concept aims to improve people, animals, plants and the environment’s health and well-being by integrating interlinked systems. The World Organisation for Animal Health has modernised its worldwide information system at global level on animal diseases (including zoonoses), a mechanism whereby all countries are linked on-line to a central server that collects all the requisite notifications sent to the OIE, covering 100 priority terrestrial and aquatic animal diseases. However, The OIE, WHO and the Food Agriculture Organization of the United Nations (FAO) have created GLEWS, the Global Early Warning System, a platform shared by the three organisations to improve early warning on animal diseases and zoonoses worldwide. At the national level, the OIE has created a contrivance whereby countries can participate to have an OIE independent judgement of their animal health system, including their Veterinary Services’ compliance with international standards of quality adopted and published by the OIE and serving as the basis for good governance. More than 120 countries have already taken this step as part of the worldwide application of the OIE PVS (Performance of Veterinary Services) tool (5). A PVS evaluation system imparts a preliminary diagnosis of governance, which can then be followed up by support in the form of a gap analysis mission to establish what “treatment” will be needed, according to the country’s own priorities, to remedy weaknesses detected during the diagnosis. Although there is not yet an equivalent system for public health systems, application of the PVS can, among its many benefits, enable recommendations to be made on ways of improving cooperation between the Veterinary Services and the Public Health Services. Recent events have shown just how important this cooperation can be in dealing with zoonotic diseases such as rabies and highly pathogenic avian influenza, and indeed with certain types of foodborne diseases. Millions of people and animals throughout the world are affected by zoonotic diseases every year. Those zoonotic diseases include Rabies, Salmonella infection, West Nile virus infection, Q Fever (Coxiella burnetii), Anthrax, Brucellosis, Lyme disease, Ringworm, Ebola etc. Similar to humans, animals are also at risk of getting sick from some diseases and environmental hazards. Because of this, they can sometimes serve as early warning signs of potential human illness. For example, birds often die of West Nile virus before people in the same area get sick with West Nile virus infection. In all these cases, controlling the pathogen at its source in animals could help to avoid subsequent public health problems, which explains the importance of suitable budgetary allocations for disease prevention and the usefulness of national joint committees with the participation of the Veterinary Services and the Medical Services, aimed at establishing permanent consultation and cooperation, a situation that unfortunately does not exist at all in too many countries. The multiple components of One Health provides policymakers and other sectors of society with the necessary tools and resources to set national priorities and improve the quality of overall health (6,7).
In spite of the efforts made by various sectors, the threat of infectious diseases outbreak is still there. Different social and environmental shocks, such as natural disasters, the lack of proper environmental hygiene and the changes in the environment’s vector ecology, have increased the number of global disease outbreaks (6). The One Health approach aims to reduce these risks through a comprehensive approach to environmental, human and animal health. As the guiding principle of the new international agreement on pandemic preparedness, One Health is also expected to play a leading role in prevention and response efforts to outbreaks, epidemics and pandemics (6,10).
Challenges
One Health issues arise due to emerging, re-emerging, and endemic zoonotic diseases, neglected tropical diseases, antimicrobial resistance, vector-borne diseases, environmental contamination, food safety and food security, climate change and other health threats shared by people, animals, and the environment. eg., Antimicrobial-resistant germs can spread quickly through communities, healthcare facilities, the food supply, and the environment (soil, water), making it harder to treat certain infections in animals and people. Vector-borne diseases are on the rise with warmer temperatures and larger mosquito and tick habitats. Diseases in food animals can threaten supplies, livelihoods, and economies. The human-animal bond can help improve mental well-being. Contamination of water used for drinking, recreation, and more can make people and animals sick. Even various chronic disease, injury, mental health, occupational health, and non-communicable diseases can benefit from a One Health approach involving collaboration across disciplines and sectors. Due to lack of proper coordination among different sectors the implementation of One Health concept is hindered in many countries. Many sectors may not effectively integrate their efforts because of a lack of resources, incongruent budgeting procedures, and limited sharing of best practices. Factors that affect the coordination of the different sectors are the allocation of resources, training and education disparities and the environment’s various fields and disciplines. (4,9). Most people rely on the primary health care system to meet their healthcare needs. So, the primary care providers have to play a vital role in the management of human health by retaining a broader environmental perspective (4). Therefore, One Health should be integrated into community-orientated care so that all relevant sectors are working together efficiently to improve the quality of healthcare. The One Health approach aims to reduce these risks through a comprehensive approach to environmental, human and animal health. As the guiding principle of the new international agreement on pandemic preparedness, One Health is also expected to play a leading role in prevention and response efforts to outbreaks, epidemics and pandemics (6,8).
Success of One Health One World Concept:
It requires the cooperation of human, animal, and environmental health partners. Professionals in human health (doctors, nurses, public health practitioners, epidemiologists), animal health (veterinarians, paraprofessionals, agricultural workers), environment (ecologists, wildlife experts), and other areas of expertise need to communicate, collaborate on, and coordinate activities. Other relevant players in a One Health approach could include law enforcement, policymakers, agriculture, communities, and even pet owners. No one person, organization, or sector can address issues at the animal-human-environment interface alone.
- Centers for Disease Control and Prevention. One Health Basics. Available online: https://www.cdc.gov/onehealth/basics/index.html(accessed on 22 April 2024).
- Horizon Europe. Work Programme 2023–2024. Food, Bioeconomy, Natural Resources, Agriculture and Environment. European Commission Decision C (2023) 2178 of 31 March. Available online: https://ec.europa.eu/info/funding-tenders/opportunities/docs/2021-2027/horizon/wp-call/2023-2024/wp-9-food-bioeconomy-natural-resources-agriculture-and-environment_horizon-2023-2024_en.pdf(accessed on 22 April 2024).
- Food and Agriculture Organization of the United Nations (FAO), World Organisation for Animal Health (OIE), United Nations Environmental Programme (UNEP), World Health Organization (WHO) . One health joint plan of action [homepage on the Internet]. 2022. [cited 2022 Oct 12]; p. 4. Available from: https://www.oie.int/en/document/one-health-joint-plan-of-action-summary/ [Google Scholar] [Ref list]
- The World Bank. One Health – Operational framework [homepage on the Internet]. 2018. [cited 2022 Oct 13]. Available from: http://documents.worldbank.org/curated/en/703711517234402168/pdf/123023-REVISED-PUBLIC-World-Bank-One-Health-Framework-2018.pdf
- Bulletin – One Health. 2009. [cited 2023 Nov 2]. Available from: https://www.woah.org/app/uploads/2021/03/bull-2009-2-eng.pdf
- Zielinski C. COP27 climate change conference: Urgent action needed for Africa and the world. Fam Med Community Health. 2022;10(4):e002012. 10.1136/fmch-2022-002012 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Mackenzie JS, Jeggo M. The One Health approach – Why is it so important? Trop Med Infect Dis. 2019;4(2):88. 10.3390/tropicalmed4020088 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
- Adisasmito WB, Almuhairi S, Behravesh CB, et al.. One Health: A new definition for a sustainable and healthy future. PLoS Pathog. 2022;18(6):e1010537.
- World Health Organization . One Health High Level Expert Panel (OHHLEP) annual report 2021. 2021. [cited 2022 Sep 28]; p. 1–35. Available from: https://www.who.int/groups/one-health-high-level-expert-panel/members [Google Scholar]