RABIES : ALL FOR ONE – ONE HEALTH FOR ONE
Ponnada Sridevi,
PhD Scholar, Department of Veterinary Anatomy
Madras Veterinary College, Chennai (TN)
Introduction
Rabies is one of the oldest recognized diseases affecting humans and one of the most important zoonotic diseases discovered and named by Girolamo Fracastoro in 15th century. The word “Rabies” has been derived from the Sanskrit word “Rabhas” which means “To do Violence“. Another belief is that, the word has originated from the Latin word “Rebere” which means “To rave“, meaning talking irrelevantly (delirium) also known as “Jalasanthra“, which means agony caused by water. The first written record of rabies is in the Mesopotamian Codex of Eshnunna (1930 BC), which dictates that the owner of a dog showing symptoms of rabies should take preventive measure against bites. Rabies was considered a scourge for its prevalence in the 19th century. In 6th July 1885, Sir Louis Pasteur for the first time successfully treated a 9 year Old boy Joseph Meister with his vaccine. Rabies is a zoonotic viral disease with a fatality rate of 100% but 100% vaccine preventable.
India has reported about 62 million stray dogs across the country. In India, Rabies is endemic in all States/UTs except Andaman and Nicobar and Lakshadweep Islands and 96% of the mortality and morbidity due to rabies is associated with dog bites. Although rabies affects people of all age groups, children are the most vulnerable which constitutes 40% of people exposed to dog bites in Rabies-endemic areas.
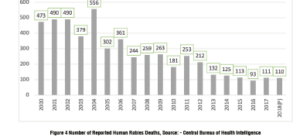
Number of reported human rabies death,source- Central Bureae of Health Intelligance
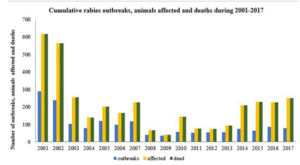
Cumulative rabies outbreak, animals affected and death during 2001- 2017
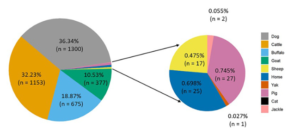
Species wise cumulative rabies cases in animals during 2001–2017 (Source: Veterinary Epidemiology Center).
Rabies is a viral infection that primarily affects mammals, including humans. It is caused by the Lyssavirus
Transmitted by common route are
- Rabies bites or scratches- most common mode of transmission is through a bite or scratch from an infected animal.
- Saliva contact – rabies can also be transmitted if the saliva from an infected animal comes into contact with mucous membranes (such as the eyes, mouth, or nose) or open wounds of a person or another animal
Transmitted by less common by inhalation, organ transplants, corneal transplants
Common Carriers of Rabies
In India, Rabies is transmitted commonly by dogs and cats (~97%), followed by wild animals (2%) such as mongoose, foxes, jackals, and wild dogs, and occasionally by horses, donkeys, monkeys, cows, goats, sheep, and pigs. Rodents, rats and bandicoots, squirrels, rabbits and birds, are generally not known to transmit Rabies.
TYPES OF RABIES VIRUS
STREET VIRUS : the virus recovered from naturally. Occurring cases of rabies
FIXED VIRUS : the virus which has a short, fixed and reproducible incubation period
INCUBATION PERIOD:
Normally 3 weeks-3 months
May be short that is 15 days or may be prolonged for years.
Depends on site of bite, Severity of bite, Richness of nerve supply, Amount of saliva deposited, Species of biting animal.
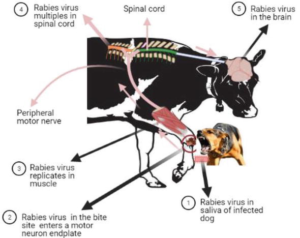
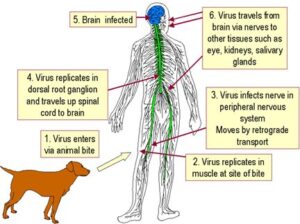
PATHOGENESIS
CLINICAL SIGNS OF RABIES IN ANIMALS AND HUMANS
In animals
Initial stage symptoms
- Restlessness- they are constantly in fear or waiting for something
- Withdrawal- animals can become very shy and start hiding away from the people spending a lot of time alone
- Licking the bite- they will often lick, scratch, sniff or even bite the infected wound
- Aggression
Advanced stage symptoms
- Furiousness- dogs can also attack their owner as if they do not recognize them anymore
- Dilated pupils
- Seizures – trembling and shanking heavily
- Lack of fear- all the innate and learned fear will disappear due to brain being cloudy from the virus
Final stage symptoms
- Salivation – excess salivation unable to fully close their mouth with the jaw drooping down
- Paralysis – spread to the other part of the body eventually leading to coma and death
In Humans
CLASSICAL HYDROPHOBIA: (80-90% of cases)
Prodromal stage: First clinical symptoms: non-specific, i.e., malaise, fever, headache, tingling and numbness at the site of bite
Stage of excitement: CNS is affected in the following order- sensory, motor and sympathetic system
Stage of paralysis
DUMB/PARALYTIC RABIES: (10-20% of cases) Seen among partially immunized person. The common clinical features include
Gradual ascending paralysis
Constipation and urinary retention
Stupor, coma and death within 1-2 weeks
Hydrophobia is usually absent
Diagnosis
- Samples-saliva, serum, spinal fluid, and skin biopsies of hair follicles at the nape of the neck
- Saliva-virus isolation or reverse transcription
- Polymerase chain reaction (PCR)
- Serum and spinal fluid-antibodies to rabies virus
- Skin biopsy specimens are examined for rabies antigen in the cutaneous nerves at the base of hair follicles.
Diagnostic tests
- Histopathology & Electron Microscopy
- Detection of antigen by taking skin biopsy using
- Direct fluorescent antibody test (DFA)
- Virus isolation from saliva & other secretions
- CSF analysis and CT scan
- ELISA
- RT-PCR- saliva & skin biopsy
- Negri bodies
- FAT
Prevention
Post-exposure prophylaxis (PEP) is a series of rabies vaccinations and, if needed, rabies immune globulin, given to individuals after a potential exposure to the virus.
Pre-exposure prophylaxis is also recommended for individuals at high risk of rabies exposure, such as veterinarians, wildlife workers, and travellers to rabies-endemic areas
- Post-exposure prophylaxis (PEP)
Post-exposure prophylaxis (PEP) is the emergency response to a rabies exposure. This prevents the virus from entering the central nervous system, which would invariably result in death. PEP consists of
- Extensive washing with water and soap for at least 15 minutes and local treatment of the wound as soon as possible after a suspected exposure
- A course of potent and effective rabies vaccine that meets WHO standards and
The administration of rabies immunoglobulin or monoclonal antibodies into the wound, if indicated
Exposure risk and indications for PEP
Depending on the severity of the contact with the suspected rabid animal, administration of a full PEP course is recommended as follows:
| Table: Categories of contact and recommended post-exposure prophylaxis (PEP) | ||
| Categories of contact with suspect rabid animal | Post-exposure prophylaxis measures | |
| Category I – touching or feeding animals, animal licks on intact skin (no exposure) | Washing of exposed skin surfaces, no PEP | |
| Category II – nibbling of uncovered skin, minor scratches or abrasions without bleeding (exposure) | Wound washing and immediate vaccination | |
| Category III – single or multiple transdermal bites or scratches, contamination of mucous membrane or broken skin with saliva from animal licks, exposures due to direct contact with bats (severe exposure) | Wound washing, immediate vaccination and administration of rabies immunoglobulin/monoclonal antibodies | |
Category II and III exposures require PEP.
WHO recommends administering rabies vaccines intradermally, as this reduces the amount of necessary vaccine and therefore the cost by 60–80% without compromising any safety or efficacy.
2.Pre-exposure prophylaxis:
Full IM dose or 0.1 ml ID dose to be given on days 0, 7 and either day 21 or 28 Laboratory staff handling the virus and infected material Clinicians, Persons attending to human rabies cases Viz. Veterinarians, Animal handlers and catchers, Wildlife wardens, Quarantine officers and travellers from rabies free areas to rabies endemic areas. Antibody titres checked every 6 months during the initial two years period after the primary vaccination. If it is less than 0.5 IU/ml a booster dose of vaccine should be given. Subsequently, sero-monitoring is recommended every two years.
- Vaccination Schedule:
Preparation for rabies typically involves a series of three or four rabies vaccinations given on specific days. The exact schedule may vary depending on the specific vaccine used. The most common schedule is on days 0, 7, and 21 or 28. An additional booster dose may be given at 1 year, and then booster doses are recommended every 2 to 5 years for ongoing protection, depending on the individual’s risk level.
- Rapidly booster the immune response to the virus.
- It provides a level of immunity that allows the individual more time to seek post-exposure prophylaxis (PEP) if they are bitten or scratched by a potentially rabid animal.
- The duration of protection from pre-exposure prophylaxis can vary among individuals. Some people may have protective immunity for several years, while others may require booster doses more frequently. Booster doses are typically recommended based on the risk of exposure.
- Public Awareness of disease transmission, especially for a potentially fatal and serious disease like rabies, is crucial for public health and safety
- Mass Vaccination of Dogs: Rabies control efforts often focus on vaccinating domestic dogs, as they are a primary source of rabies transmission to humans. Mass vaccination campaigns aim to increase the coverage of vaccinated dogs in at-risk areas
- Animal Birth Control (ABC) programmes for dog population management.
MILLSTONES OF RABIES CONTROL EFFECTS IN INDIA

Rabies is included in WHO’s 2021–2030 Roadmap for the global control of neglected tropical diseases, which sets regional, progressive targets for the elimination of targeted diseases. Rabies is one of these. As a zoonotic disease, it requires close cross-sectoral coordination at the national, regional and global levels.
As per WHO estimates, globally, there are 59,000 human deaths due to dog-mediated rabies. India contributes to one third of the total global burden due to rabies and two-third of rabies burden in the South East Asia Region as per the WHO-APCRI 2004 Survey. In 2015, the world called for action by setting a goal of “Zero human deaths due to dog-mediated rabies by 2030”, worldwide. Subsequently, four organizations the World Health Organization (WHO), the World Organization for Animal Health (OIE), the Food and Agriculture Organization of the United Nations (FAO), and the Global Alliance for Rabies Control (GARC) – have joined forces, as the United Against Rabies collaboration, and determined to reach the global target of “Zero human deaths due to dog-mediated Rabies by 2030”. Countries like Western Europe, Canada, the US, Mexico, Japan & Latin America have already eliminated dog-mediated Rabies through successful canine rabies vaccination and One health approach.
Five pillars for the elimination of rabies
- Socio- cultural
Rabies control involves a wide range of stakeholders including the general public. The socio-cultural context influences rabies perceptions and dog- keeping practices of at-risk populations. Understanding the context guides approaches to motivate behavioural change and plan feasible delivery of services.
- Awareness: build awareness of dog-mediated rabies as a preventable global public health problem including through participation in initiatives such as World Rabies Day and the End Rabies Now campaign
- Responsible dog ownership: promote responsible dog ownership and dog population management practices, including dog vaccination, in accordance with OIE standards
- Bite prevention and treatment: develop and implement education programmes on bite prevention and first aid for both children and adults
- Post-exposure prophylaxis: increase awareness and understanding of post- exposure prophylaxis (PEP) imperatives and options including intradermal administration
- Community engagement: encourage community involvement and engagement in activities to eliminate dog-mediated rabies
2.Technical
Effective animal health and public health systems are required to eliminate dog- mediated human rabies. These systems must be strengthened and resourced appropriately, and gaps identified and filled.
- Vaccination: ensure safe, efficacious and accessible dog and human vaccines and immunoglobulins, and promote and implement mass dog vaccination as the most cost-effective intervention to achieve dog-mediated human rabies elimination
- Logistics: collect data on needs forecasts to inform the vaccine procurement system and to create and sustain the logistics and infrastructure required for effective delivery and implementation of mass dog vaccination programmes and PEP administration
- Diagnostics: ensure capacity and capability for rapid and accurate rabies diagnosis through accessible, well equipped laboratories and trained personnel
- Surveillance: support improved surveillance, sampling, reporting, and data-sharing Technical support: provide guidance and technical support for the development and tailoring of regional and national plans, including promoting the use of existing tools
- Proof of concept: support proof-of- concept programmes, and then scale up through leveraging of success
3.Organization
The One Health approach of close collaboration is applied. Leadership, partnership and coordination for rabies elimination activities arise from the human health and animal health sectors and other stakeholders.
- One Health: promote the One Health approach and intersectoral coordination through national and regional networks
- Good governance: establish good governance, including clear roles, chain of command, measurable outcomes and timelines
- Harmonization: align work plans and activities with national and regional priorities and approaches fostering synergies among sectors
- Coordination: coordinate and combine human resources, logistics and infrastructure of other programmes and initiatives, as appropriate and feasible
- Indicators and performance: identify targets and their indicators to support performance measurement, including surveillance and validation data, to identify areas requiring attention or extra support
- Monitoring and evaluation: support monitoring and evaluation of national plans to ensure timely and cost effective delivery
4.Political
Success depends on political will and support for elimination of dog-mediated human rabies. Political will results from recognition of rabies elimination as a national, regional and global public good
- Political support: political support is essential and most relevant during and following country instability
- International support: encourage countries to request a resolution on dog-mediated human rabies elimination through the World Health Assembly (WHO) and the General Assembly of Delegates (OIE)
- Legal frameworks: establish and enforce appropriate legal frameworks for rabies notification and elimination
- Demonstrating impacts: demonstrate the compelling case for mass dog vaccination programmes and their impact on protecting and saving human lives
- Regional engagement support active national and regional engagement and cooperation to commit to a rabies elimination programme and promote the exchange of lessons learnt and experiences to leverage resources and engagements
5.Resources
Rabies elimination activities frequently span several years and therefore require sustained, long-term support.
- Case for investment: promote the case for investment in dog-mediated human rabies elimination to persuade countries, policy makers and donors of the feasibility, merit and value of investing in rabies elimination strategies
- Business plans: prepare business plans based on the Global Framework for Dog-mediated Human Rabies Elimination
- Investment: encourage different forms of investment and partnerships to leverage resources and engagement
One Health approach

Model framework for coordinated One Health approach to control rabies in South Asia
Conclusion:
The one health approach is still a highly integrated research effort that involves cross-sectoral collaboration from human, animal, and environmental health disciplines at local, national, and international levels. This approach focuses on thorough, strategic, and targeted control and prevention, and collaboration between veterinarians, clinicians, epidemiologists has a crucial role to play in raising public awareness about the preventive measures for zoonotic infections in animal and enabling early outbreak detection to ensure safe health and a better world.