ROLE OF CALCIUM & ITS SUPPLEMENTATION TIPS TO DAIRY CATTLE
Compiled & edited by-DR. RAJESH KUMAR SINGH, (LIVESTOCK & POULTRY CONSULTANT), JAMSHEDPUR, JHARKHAND,INDIA 9431309542, rajeshsinghvet@gmail.com
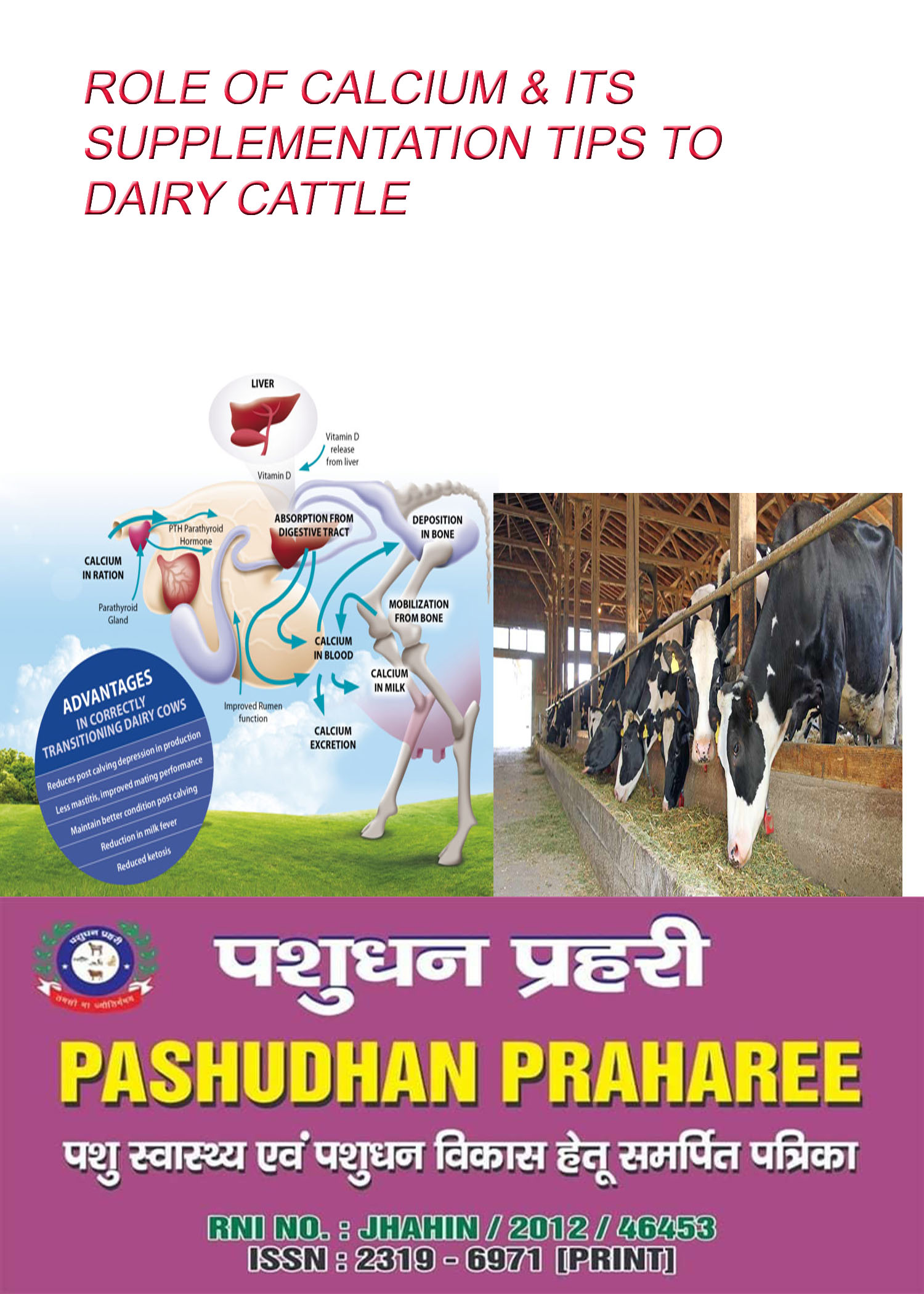
Calcium is primarily needed for bones, teeth, nerves, muscles, blood clotting, and body enzymes. Milk contains a large amount of calcium. 98% of the cow’s body calcium is found in the bone. Blood calcium levels are critically important to the cow’s health. Therefore, this level is tightly controlled by the cow’s endocrine system, specifically the parathyroid gland. When the parathyroid gland recognizes that blood calcium is low, calcium reserves are mobilized from the bone and intestinal calcium absorption is increased from the diet. Unfortunately, rapid significant drops in blood calcium cannot always be counteracted by these mechanisms. The result is milk fever.
Ca Homeostasis ———
Blood Ca in the adult cow is maintained around 2.1–2.5 mmol/L. In order to prevent blood Ca from decreasing at the onset of lactation, which has a variety of severe consequences to life processes beyond parturient paresis, the cow must replace Ca lost to milk by withdrawing Ca from bone or by increasing the absorption of dietary Ca. While this is potentially damaging to bones (lactational osteoporosis typically results in loss of 0.09–0.13 of skeletal Ca in dairy cows, which is reversible in later lactation), the main objective – to maintain normocalcemia – can be achieved. Bone Ca mobilization is regulated by parathyroid hormone (PTH), which is produced whenever there is a decline in blood Ca. Renal tubular reabsorption of Ca is also enhanced by PTH. However, the total amount of Ca that can be recovered by reducing urinary Ca excretion is relatively small. A second hormone, 1,25-dihydroxyvitamin D, is required to stimulate the intestine to efficiently absorb dietary Ca. This hormone is made within the kidney from Vitamin D in response to an increase in blood PTH. Put simply, hypocalcemia and milk fever occur when cattle do not extract enough Ca from their bones and diet to replace the Ca lost to milk. Several nutritional factors are involved in the breakdown of Ca homeostasis that results in milk fever.
Types of calcium ————
There are four commonly used types of calcium salts that can be used in the construction of calcium boluses: calcium chloride, calcium sulfate, calcium propionate and calcium carbonate. Each type has its own benefits and risks. Calcium boluses are usually comprised of several types of calcium salts that have different solubilities in the rumen, .
“The primary site for calcium absorption in the cow is in the small intestine, with the rumen considered a secondary site,” he says. “The main workhorse in most of these calcium boluses is calcium chloride. A calcium bolus that is based on calcium chloride will raise blood calcium about the same as giving half a bottle of calcium intravenously.”
Calcium chloride is highly soluble in the rumen and can create a high enough concentration of ionized calcium to allow for passive transfer of calcium through the ruminal wall, which produces a rapid rise in blood calcium. Calcium chloride also creates metabolic acidosis, which will increase calcium resorption from bone.
On the other hand, calcium chloride is quickly available and rapidly absorbed. Therefore, it does not provide calcium over long durations.
Calcium carbonate has good bioavailability after it is dissolved in the acidic environment of the abomasum and is available for a longer duration.
Calcium sulfate is a source that contributes to blood acidity when it is absorbed from the cow’s gastrointestinal tract. This acidity helps a cows’ parathyroid hormone function. Calcium sulfate also dissociates at a slower rate than calcium chloride. This characteristic makes calcium sulfate complementary to other sources.
Calcium propionate requires the administration of a significantly greater volume to provide the same amount of calcium when compared to calcium chloride.
“Calcium propionate is a wonderful calcium and energy source for a fresh animal,”
FAQ ON CALCIUM FEEDING TO DAIRY CATTLE BY -Dr. Garrett R. Oetzel, University of Wisconsin
When is hypocalcemia the most prevalent?
The start of lactation challenges Ca homeostasis (balance) in the dairy cow. There is a sudden loss of Ca from the blood into the colostrum at the time of calving. It takes 3 to 4 days for Ca to start being mobilized from the bone into the blood stream. During that time period cows are at increased risk for subclinical hypocalcemia.
What are the key risk factors for hypocalcemia?
1) Increasing parity (lactation number) increases the risk for hypocalcemia because the loss of Ca resorption capacity from the bone is linked to declining skeletal growth. First lactation cows are at low risk for subclinical hypocalcemia because they are still growing and the bone still has good resorption capability, therefore, they are able to mobilize Ca easier than older cows.
2) Increasing milk yield increases the risk for hypocalcemia because colostrum production increases thus increasing the amount of Ca removed from the blood stream at parturition.
Why is there a concern about low blood Ca if a cow is not showing clinical signs of hypocalcemia?
Calcium is the highest priority mineral. It is essential for muscle and nerve function. It is involved in skeletal muscle strength, GI motility (smooth muscle function), and is also important in immune function. Subclinical hypocalcemia increases the risk for certain metabolic diseases (increased risk for metritis, ketosis, displaced abomasum (DA), and decreases immune function) thus increasing the risk that an individual cow may be removed from the herd.
How can subclinical hypocalcemia be prevented or minimized?
There are 2 primary methods of prevention for subclinical hypocalcemia (diet and oral supplementation of Ca). Nutritional strategies that have been found to be effective in reducing the incidences of hypocalcemia included;
1) low Ca diets prepartum,
2) dietary acidification prepartum
3) increased Mg in the prepartum diet
These nutritional strategies have been shown to be beneficial in reducing the incidences of hypocalcemia, but subclinical hypocalcemia cannot be prevented through diet alone (Oetzel). Oral Ca supplementation has been found to be effective in reducing the incidences of subclinical hypocalcemia especially when used in combination with nutritional strategies. Cows absorb oral Ca rapidly and sustain increased blood level Ca for 4 to 6 hours. There are different types of oral Ca supplementation. Calcium chloride and calcium sulfate invoke an acidogenic response in cows which will cause the cow to mobilize more Ca from her skeleton. Oetzel recommends giving two doses, about 12 hours apart. Give the oral Ca bolus at calving (if the cow is not ‘down’) and another bolus 12 hours later to give a sustained improvement in blood Ca levels.
What are some successful oral Ca strategies for cows?
Oetzel states not to give oral Ca to down cows. Oral Ca supplements do work for early milk fever cases (before the cow goes down), after successful treatment of down cows, for off-feed cows (especially early lactation), and to cows with impaired intestinal motility (subacute ruminal acidosis).
When do you use IV instead of oral calcium?
If a cow is ‘down (recumbent)’ because of clinical hypocalcemia (milk fever; <4 mg/dL of Ca in blood), Oetzel recommends giving a bottle of Ca borogluconate via IV infusion. Down cows can quickly suffer irreversible musculo-skeletal damage. The IV delivers 10.5 grams of Ca directly into the blood which causes a massive spike in blood Ca, and will help many cows recover quickly from milk fever. However, there can be some side effects from elevating blood Ca so high. Occasionally, a cow will die from cardiac arrest when a bottle of Ca is given because when blood Ca concentrations are at or above 20 mg/dL there is an increased risk of cardiac arrest (because of this threshold, it is never recommended to give a second bottle of Ca with the initial IV treatment). Secondly, some of the cows that were given a bottle of Ca for clinical hypocalcemia will relapse with another case of clinical milk fever and need another bottle of Ca. Oetzel suspects this is due to what he terms the ‘Calcitonin Response’, where the spike in blood Ca from the IV signals the hormone calcitonin to release. Calcitonin does not allow Ca to mobilize from the bone, therefore the blood Ca levels end up dropping lower than the normal cows.
Oetzel’s
TIPS FOR CALCIUM FEEDING:—-
1. Don’t give oral calcium to a down cow.
2. Don’t give IV calcium to a standing cow.
3. Clinical hypocalcemia (down cows; blood Ca <4 mg/dL): Use both IV and oral forms of Ca treatment.
1. Initially, give IV of Ca
2. Followed by 2 oral Ca boluses.
3. Give the 1st Ca bolus 12 hours after IV injection and the 2nd Ca bolus 12 hours later.
4. Give oral Ca to 2nd and greater lactation cows (Don’t give to 1st lactation cows)
5. Subclinical hypocalcemia (≤8.6 mg/dL in blood the day of calving): Use both nutritional intervention and oral Ca supplements.
1. The nutritional intervention usually happens during the prepartum period.
2. Give 1 oral Ca bolus at calving followed by another oral Ca bolus 12 hours later.
6. If the dairy only wants to give 1 bolus (which Dr. Oetzel wasn’t recommending) give it the day after calving
7. If you give oral Ca around calving give CaCl2 (do not give drench buckets such as calcium propionate because the glucose suppresses appetite by signaling the cow is full).
8. 36 hours after calving it is okay to give the drench bucket (Ca with glucose).
Oral Ca treatments at calving—–
Ca administered to the fresh cow may arguably be called a treatment rather than a preventative measure for hypocalcemia. Contrasts between the effects observed with intravenous, subcutaneous, and oral Ca treatments have been described elsewhere (Goff, 1999). Briefly, the concept behind oral supplementation is that the cow’s ability to utilize active transport of Ca across intestinal cells is inadequate to help her maintain normal blood Ca concentrations. By dosing the animal with large amounts of very soluble Ca it is possible to force Ca across the intestinal tract by means of passive diffusion between, not across, intestinal epithelial cells. Best results are obtained with doses of Ca between 50 and 125 g Ca/dose. Ca chloride has been used but can be caustic. Large or repeated doses of calcium chloride can induce an uncompensated metabolic acidosis in the cow, especially if the cow is already being fed an acidogenic diet (Goff and Horst, 1993). Ca propionate is less injurious to tissues and is not acidogenic. It has the added benefit of supplying propionate, a gluconeogenic precursor Goff and Horst, 1993; Pehrson et al., 1998). For best control of hypocalcemia a dose is given at calving and again 24 h later. Larger or more frequent dosing can be toxic. Toxic doses of Ca can be delivered orally—about 250 g Ca in a soluble form will kill some cows (Goff et al., 2002). The benefit of adding oral Ca on top of a properly formulated low DCAD program does not seem to warrant the added expense

Reference-on request