Surra in Domestic Animals – A Zoonotic Diseases
Surra, caused by the protozoan parasite Trypanosoma evansi, is a significant parasitic disease affecting domestic animals with potential zoonotic implications. While predominantly recognized as a disease of livestock, surra poses a threat to human health due to its zoonotic nature. In this article, we will explore the characteristics of surra, its impact on domestic animals, and the potential risks associated with zoonotic transmission.
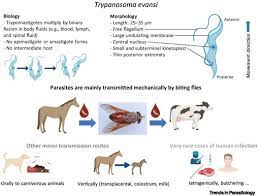
Surra is caused by a parasitic protozoan Trypanosoma evansi. The disease affects mainly camels and horses, but buffaloes and cattle are also affected. Trypanosomes infect a variety of hosts and cause various diseases, including the fatal human diseases sleeping sickness, caused by Trypanosoma brucei, and Chagas disease, caused by Trypanosoma cruzi. The incidence of surra increases significantly during the rainy season when there are large biting fly populations. The losses are due to reduced productivity, mortality and cost of treatment.
Human Trypanosomiasis in India: Is it an emerging new zoonosis?
Trypanosomes are flagellated protozoan parasites infecting man (human trypanosomiasis) and a wide range of animals (animal trypanosomiasis). Human trypanosomiasis is confined to Sub-Saharan Africa and Latin America and exists in two forms: 1. Human African trypanosomiasis (HAT) (sleeping sickness) is endemic in Sub-Saharan Africa. It is a dreadful fatal disease and was responsible for devastating epidemics in 1920s, with resurgence in 1990s. It is caused by Trypanosoma brucei gambiense (chronic form) or Trypanosoma brucei rhodesiense (acute form) and 2. American trypanosomiasis (Chagas disease) caused by T. cruzi is endemic in Latin America. Both diseases are transmitted by vectors: Human African Trypanosomiasis by infected saliva of Tsetse fly, and chagas by infected feces of bugs. Though human infection by animal species is “not possible” because of a trypanolytic factor in human serum, there are several reports of atypical human infection caused by animal trypanosomes, such as T.evansi, T. lewisi and T. congolense, especially from India. A new form of human trypanosomiasis has emerged with the first human case in the world caused by T. evansi. T. evansi– identified for the first time in horses and camels in 1881 in the Punjab region (India) by Griffith Evans, an English veterinary surgeon–causes disease in animals called “surra” which is commonly found not only in livestock in India, but has a worldwide distribution . Authors reported the first confirmed case of human trypanosomiasis caused by T. evansi in a farmer from Seoni village, near Nagpur in 2005. Nineteen atypical human cases of trypanosomiasis caused by animal trypanosomes are reported: 8 to T. lewisi, 5 to T. evansi and 4 of them are due to T. brucei, one to T. vivax, one to T. congolense and T. brucei species. All cases due to T. lewisi were observed in Asia. Out of 19 cases, 6 are infants and 8 are from India. Two more cases have very recently been detected in Puducherry (unpublished). Particularly in the State of Maharashtra the concern is more serious because one case of T. evansi and two cases of T. lewisi have been reported in a span of 3 years. The environmental conditions in India are conducive to the spread of the parasite from animals to human beings.
Animal trypanosomiasis
In contrast to human trypanosomiasis, animal trypano-somiasis has a worldwide distribution and is common in India. India has the unique distinction of being the country where the first two mammalian trypanosomes, i.e. Trypanosoma lewisi and T. evansi were discovered. T. lewisi is a natural parasite of rats while T. evansi is a pathogenic species of number of domesticated animals like cattle horses and causes a disease called “surra” in animals. High prevalence of these two animal trypanosomes in India is now a matter of concern.
Transmission
Mechanical transmission occurs most importantly by horse fly (Tabanus spp.), followed by stable fly (Stomoxys spp). Transmission is enhanced when horses or camels are closely tied up, when they have high numbers of parasites in their blood. Indigenous cattle, buffalo, and several species of wild life may act as reservoir of infection for horses and camels.
Clinical signs
The main clinical findings are intermittent fever, progressive anemia, edema of dependent parts of the body, urticaria, dullness, listlessness, loss of body condition despite a good appetite, disappearance of hump and atrophy of thigh muscles, weakness, and rough coat, nasal and ocular discharge, pin-point hemorrhages of the mucous membranes and often around the eyelids, nostrils and anus may be present. Terminally, nervous signs may be seen, like paraplegia, paralysis, delirium, and convulsion. Surra is invariably fatal in camels and horses, but camels may exhibit chronic signs for years. These signs include a reduction in milk yield and capacity for work, and a high abortion rate in pregnant females. Camels with chronic surra become more prone to infection with other diseases; it is usually associated with mange and pneumonia. In endemic areas, cattle and buffalo usually have mild infections which may be exacerbated by stress from adverse climatic conditions, work, or inter current disease. Signs may include irregular estrus, abortion, and stillbirth in cows and poor semen quality in bulls. There may be enlarged lymph nodes and internal organs. Haemolytic anaemia is a characteristic sign. A more severe disease in cattle is characterized by nervous signs and high mortality rate. The signs include circling, excitation, jumping, aggressive behavior, lateral recumbency, convulsion and finally death. In general, T. evansi is only slightly pathogenic for sheep, goats and pigs, although occasional outbreaks of disease may occur in pigs. Carnivores are highly susceptible to acute infection; the disease is characterized by well-marked edema, particularly in the scrotum, ears, and neck. Opacity of the cornea is frequently present, emaciation is rapid and death can occur within 2 weeks. Dogs occasionally exhibit nervous signs suggestive of rabies.
Lesions
- There are no pathognomonic gross and microscopic lesions.
- · The carcass is emaciated, pale and may be icteric.
- · Edema is evident, ascites and hydrothorax may be present.
- · In acute, fatal cases, there may be extensive petechiation of the serosal membranes, especially in the peritoneal cavity.
- · Enlargement of lymph nodes and spleen.
- · Trypanosomes are detected in all tissues and body fluids of fresh carcass · In chronic cases, swollen lymph nodes, serous atrophy of fat, and anemia are seen.
- · Presence of blood in the cerebrospinal fluid (CSF) is evidence of CNS involvement.
Diagnosis
- A presumptive diagnosis is based on finding an anemic animal in poor condition in an endemic area.
- · Confirmation depends on demonstrating trypanosomes in stained blood smears or wet mounts.
- · In wet mounts, motile organisms may be visible in the buffy coat when a blood sample is centrifuged.
- · Other infections that cause anemia and weight loss, such as babesiosis, anaplasmosis and haemonchosis, should be ruled out by examining a stained blood smear.
- · Various serologic tests can be done to measure antibody to trypanosomes.
Treatment
- Consult veterinarian for treatment.
- · Several drugs like Quinapyramine sulphate, Melarsomine dichlorhydrate and suramin can be used for treatment.
- · Drug resistance can occur and should be considered in refractory cases.
Control Measures
- Fly control by aerial and ground spraying of insecticides on fly-breeding areas.
- · Detection and treatment of infected animals, prophylactic treatment of susceptible animals and their protection from biting flies.
- · Reduction of the reservoirs of infection.
- · Drug resistance must be carefully monitored by frequent blood examinations for trypanosomes in treated animals.
- · The use of breeds showing innate resistance to trypanosomosis should be considered.
Surra in Domestic Animals
- Causative Agent: Trypanosoma evansi
Surra is caused by Trypanosoma evansi, a protozoan parasite belonging to the genus Trypanosoma. Unlike other trypanosomes that primarily infect the blood, T. evansi can infect various tissues and organs, leading to a range of clinical manifestations.
- Transmission
The primary mode of transmission is through the bite of mechanical vectors, such as horseflies, deerflies, and other blood-sucking insects. Infected animals serve as reservoir hosts, and the parasites can be transmitted mechanically by biting insects from infected to susceptible hosts.
- Clinical Signs in Domestic Animals
Clinical signs of surra in domestic animals may include:
- Fever: Sudden onset of high fever.
- Anemia: Due to the destruction of red blood cells.
- Weight Loss: Progressive emaciation and loss of body condition.
- Edema: Swelling, particularly in the limbs and abdomen.
- Neurological Signs: Incoordination, paralysis, and central nervous system disturbances.
- Species Affected
Surra affects a wide range of domestic animals, including:
- Horses and Equids
- Cattle
- Camels
- Buffaloes
- Dogs
- Pigs
- Sheep and Goats
Zoonotic Implications
While surra is primarily considered a disease of animals, there is evidence to suggest potential zoonotic transmission. The zoonotic potential is particularly concerning in regions where surra is endemic, and close contact between humans and infected animals is common.
- Human Infections
Human infections with Trypanosoma evansi are rare but have been reported. The clinical manifestations in humans may range from asymptomatic cases to more severe conditions resembling the clinical features observed in infected animals.
- Occupational Risk
Individuals involved in activities such as veterinary care, animal husbandry, and agriculture are at an increased risk of exposure to T. evansi. Accidental contact with contaminated blood or tissues, through injuries or mucous membrane exposure, can pose a risk of zoonotic transmission.
- Diagnosis and Surveillance
Zoonotic transmission of surra emphasizes the importance of accurate diagnosis and surveillance in both animals and humans. Laboratory techniques, such as polymerase chain reaction (PCR) and serological tests, are essential for confirming infections and monitoring the prevalence of the parasite.
Prevention and Control
Preventing and controlling surra require a multi-faceted approach:
- Vector Control
Efforts to control mechanical vectors, such as implementing insecticide application and environmental management practices, are crucial for reducing transmission risk.
- Quarantine Measures
Quarantine measures are essential to prevent the introduction of infected animals into non-endemic areas. This includes screening and testing animals before transportation.
- Treatment and Chemoprophylaxis
Treatment of infected animals with trypanocidal drugs is a key component of disease control. Additionally, chemoprophylaxis in high-risk areas may be considered to prevent the spread of the parasite.
- Public Awareness and Education
Educating communities, veterinarians, and healthcare professionals about the risks associated with surra and the importance of preventive measures is vital for zoonotic disease control.
Conclusion
Surra, a parasitic disease affecting a broad spectrum of domestic animals, presents a notable zoonotic threat. The potential for human infections underscores the importance of comprehensive strategies for disease prevention, vector control, and awareness. Collaboration between veterinary and public health authorities, along with research efforts to better understand the zoonotic aspects of surra, is crucial for mitigating the impact of this disease on both animal and human populations. As global interactions and movements increase, recognizing and addressing zoonotic diseases like surra becomes imperative for the well-being of both humans and the animals we share our environments with. It is imperative that the possibility of human infection by animal trypanosomes, which has the potential to emerge as a new zoonosis, needs to be taken seriously and given more attention. Further investigations in the field and laboratory are warranted. Livestock should also be handled with care to minimize accidental infection.
Compiled & Shared by- This paper is a compilation of groupwork provided by the
Team, LITD (Livestock Institute of Training & Development)
Image-Courtesy-Google
Reference-On Request.