THEILERIOSIS IN DAIRY CATTLE:A KEY NOTE
Dr.Rakesh kr Singh, TVO, Motihari, Bihar
- • Theileriosis is an important disease in exotic and cross bred dairy cattle
AETIOLOGY
• Classification of the causative agent
•
• Genus Theileria, Family Theileriidae, Order Piroplasmida, Subclass Piroplasmia, Phylum Apicomplexa.
•
• • Theileriae are obligate intracellular protozoan parasites that infect both wild and domestic
Bovidae throughout much of the world]
• • Some species also infect small ruminants
• • They are transmitted by ixodid ticks, and have complex life cycles in both vertebrate and invertebrate hosts
• • There are six identified Theileria spp. that infects cattle; the two most pathogenic and economically important are T. parva and T. annulata
• • T. parva occurs in Eastern and Southern Africa and causes East Coast fever (ECF or Corridor
disease)
• • T. annulata causes tropical theileriosis (TT), also known as Mediterranean theileriosis and occurs
in North Africa, southern Europe and Asia
• • T. lestoquardi (T. hirci) is the only species of economic significance infecting small ruminants, and
it occurs in the Mediterranean basin, North Africa and Asia
• • Most theileriae are confined to Asia or Africa corresponding to the geographical distribution of
their vector ticks, except for the worldwide distribution of the apathogenic T. buffeli.
• Resistance to physical and chemical action
•
• Temperature: Not applicable.
• pH: Not applicable.
• Disinfectants: Not applicable.
• Survival: Theileriae are obligate intracellular protozoan parasites.
•
• EPIDEMIOLOGY
•
• Hosts
•
• • T. parva infects cattle, African buffalo (Syncerus caffer), Indian water buffalo (Bubalus bubalis),
and waterbuck (Kobus spp.)
• • Taurine breeds of cattle are generally more susceptible to ECF than zebu (Bos indicus) or sanga
breeds. In addition, introduced cattle, whether of a taurine, zebu, or sanga breed, are much more
susceptible to theileriosis than cattle from endemic areas
• • Subclinical infections are common only in cattle and water buffalo; African buffalo and waterbuck
are reservoirs for the infection
• • T. annulata infects cattle and yak (Bos grunniens), with milder infections usually seen in water
buffalo; the water buffalo is considered to be the natural host in which the parasite evolved.
• • The taurine breeds of cattle, introduced into endemic areas, have a much more severe form of
the disease than do indigenous zebu cattle
• Transmission
•
• • Both T. parva and T. annulata are spread by ticks
• • The most important vector for T. parva is Rhipicephalus appendiculatus. R. zambeziensis in
southern Africa and R. duttoni in Angola can also spread East Coast fever. T annulata is
transmitted by ticks of the genus Hyalomma
• • Ticks can remain infected on the pasture for up to 2 years depending on the climatic conditions.
• • Disease is not maintained in the absence of these field vectors.
• • Theileria sporozoites are transmitted to susceptible animals in the saliva of the feeding tick
•
Ordinarily, T. parva and T. annulata only mature and enter the saliva after the tick attaches to a
host; usually, a tick must be attached for 48-72 hours before it becomes infective; however, if
environmental temperatures are high, infective sporozoites can develop in ticks on the ground
and may enter the host within hours of attachment
• • Transovarial transmission does not occur with either T. parva or T. annulata.
• • Inside the host, Theileria sporozoites undergo a complex life cycle involving the replication of
schizonts in leukocytes and piroplasms in erythrocytes
• • Cattle that recover from Theileria infections usually become carriers
• MODE OF TRANSMISSION
•
• The disease is mostly observed during summer and rainy seasons.
• This preponderance is attributed to higher activity of vector during this season (May to October). This is also influenced by stress due to hot and humid weathers.
• The disease is transmitted by the bite of the ticks of the genus Hyalomma.
• Erythrocytic forms of the parasite are ingested by the larval and nymphal stages of the tick along with blood, while feeding on an infected animal.
• The subsequent stages of the tick (nymph and/or adults) transmit the disease during their feeding on susceptible hosts (Transtadial transmission).
• The disease can also be transmitted mechanically by inoculation of infective blood and tissue suspension made from spleen, lymph node and liver of infected animals.
• Sources of the agent
• • Sporozoites in salivary glands of infected Rhipicephalus appendiculatus (ECF) and Hyalomma
• (TT) ticks
• • Schizonts occur in spleen, lymph nodes and whole blood (lymphoblast’s) from ECF infected animals, but experimental transmission to cattle is erratic
• o Schizonts occur in spleen, lymph nodes, liver and whole blood (mononuclear cells) from
TT infected animals, and transmission by inoculated schizonts occurs readily to cattle
• Occurrence
• East Coast fever is found from southern Sudan to South Africa and west to the eastern part of the
Democratic Republic of Congo. The tick vectors can be found from sea level to over 8000 feet, in any area
where the annual rainfall exceeds 20 inches. Tropical theileriosis is seen in North Africa, southern Europe,
and the southern republics of the former USSR, the Indian subcontinent, China, and the Middle East.
• DIAGNOSIS
• Agent Identification
• • Indirect fluorescent antibody (IFA) test •
Molecular tests
•
• • Theileriosis should be suspected in tick-infested animals with a fever and enlarged lymph nodes
• • In endemic areas, the mortality rate may be high only in calves
• In the field, diagnosis is usually achieved by finding Theileria parasites in Giemsa-stained blood smears and lymph node needle biopsy smears, but species specific diagnosis is difficult as most theilerial piroplasms are morphological identical except for T. velifera. Schizonts are not always present in the superficial lymph nodes during the disease course
• Laboratory confirmation is essential
• • The incubation period for ECF is 8-12 days on average and for TT is 10-25 days
• • Morbidity and mortality vary with the host’s susceptibility and the strain of the parasite
• o The mortality rate from East Coast fever can be up to 100% in cattle from non-endemic
areas, however, in indigenous zebu cattle in endemic areas, mortality is usually low even with a morbidity of approximately 100%
• o The mortality rate for tropical theileriosis can also vary from 3% to nearly 90%,
• depending on the strain of parasite and the susceptibility of the animals
• SYMPTOMS-
• High rise of temperature (40.5˙C to 41.5˙C).
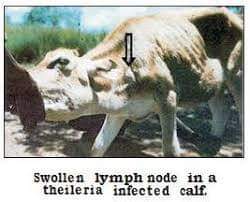
• Enlargement of regional superficial lymph nodes.
• Anorexia, restlessness and rough coat.
• Tense eye balls along with watery lacrymation.
• Laboured respiration, serous, nasal discharge and coughing.
• Depression and petechial haemorrhages on conjunctiva.
• Declination of fever and development of anaemia with high coloured urine in later stage.
• Urticarial type skin lesions.
Weakness, prostration and death
• Clinical diagnosis
•
• • The first clinical sign of ECF is usually a swelling of the draining lymph node, usually the parotid,for the ear is the preferred feeding site of the vector; this is followed by a generalised lymphadenopathy in which superficial lymph nodes such as the parotid, prescapular, and prefemoral lymph nodes, can easily be seen and palpated
• Fever ensues and continues throughout the course of infection; this rise in temperature is rapid and may reach 106°F (42°C)
• There is marked petechial and ecchymotic haemorrhage on most mucous membranes of the conjunctiva and the buccal cavity
• Anorexia develops, and loss of condition follows
• • Other clinical signs may include lacrimation, corneal opacity, nasal discharge, terminal dyspnoea, and diarrhoea
• • Before death the animal is usually recumbent, the temperature falls, and there is a severe dyspnoea due to pulmonary oedema that is frequently seen as a frothy nasal discharge
• • Mortality in fully susceptible cattle can be nearly 100%
• • The severity and time course of the disease depend on, among other factors, the magnitude of the infected tick challenge (ECF is a dose-dependent disease), and on the strain of parasites
• • Some stocks of parasites cause a chronic wasting disease
• • In recovered cattle, chronic disease problems can occur that result in stunted growth in calves and lack of productivity in adult cattle, however, this syndrome tends to be in the minority of recovered clinical cases
• • In a majority of cases, subclinical carriers can be recognised with apparently little or no effect on their productivity
• • A fatal condition called ‘turning sickness’ is associated with the blocking of brain capillaries by infected cells and results in neurological signs
• • Tropical theileriosis resembles East Coast fever, but jaundice and anaemia may also occur
• • In the acute disease of tropical theileriosis, death occurs 15-25 days after infection
• • Clinical signs might include pale mucous membranes (anaemia) or jaundice, as the piroplasms will precipitate destruction of red blood cells
• • During the stage when there is great production of macroschizonts within macrophages, there could be enlarged lymph nodes, and a generalised loss of condition and muscle wasting due to massive release of cytokines from infected cells
• • Haemorrhagic diarrhoea may be present in the terminal stages
• Lesions
A frothy exudate is frequently seen around the nostrils of an ECF-infected animal
• • Signs of diarrhoea, emaciation, and dehydration may be seen
• • Lymph nodes are greatly enlarged and may be hyperplastic, haemorrhagic, and oedematous
• • In acute cases of ECF, lymph nodes are oedematous and hyperaemic, but often become necrotic and shrunken in more chronic disease
• • Generally, muscles and fat appear normal, but depending on relative acuteness of infection, fat may become greatly depleted
• • Serosal surfaces have extensive petechial and ecchymotic haemorrhages, and serous fluids may be present in body cavities
• • Haemorrhages and ulceration may be seen throughout the gastrointestinal tract – particularly in the pyloris part of the abomasum, where necrosis of Peyer’s patches can be observed
• • Lymphoid cellular infiltrations appear in the liver and kidney as white foci
• • The most striking changes are seen in the lungs; in most cases of ECF, interlobular emphysema and severe pulmonary oedema appear, the lungs are reddened and filled with fluid and the trachea and bronchi are filled with fluid and froth
• • There are no specific lesions associated with tropical theileriosis
• • Shortly after infection, the lymph node draining the site of the tick bite will be enlarged
• • At the time of severe clinical disease or death, anaemia, jaundice, enlarged lymph nodes, muscle wasting, pulmonary oedema, and haemorrhagic enterocolitis may all be present
• • Unlike East Coast fever, which is characterised by a marked lymph proliferative response due to massive infection of lymphocytes, tropical theileriosis is primarily a macrophage infection
• o It is thought that extensive infection of macrophages stimulates a huge outpouring of
cytokines, predominantly TNFα, which accounts for many of the lesions seen
• o Macroschizonts may be seen in infected macrophage type cells within various organs
•
• Differential diagnosis
•
• • Heartwater
• • Trypanosomosis
• • Babesiosis
• • Anaplasmosis
• • Malignant catarrhal fever
• • Contagious bovine pleuropneumoniae
• • The parasites must also be differentiated from other species of Theileria.
• Laboratory diagnosis
• • In live animals, theileriosis is diagnosed by the identification of schizonts in thin smears from blood, lymph node
• • At necropsy, schizonts may be found in impression smears from most internal organs
• • Piroplasms can sometimes be found in the blood of carrier animals
• • Polymerase chain reaction (PCR) tests and DNA probes are sometimes used to detect and identify Theileria species
• • Antibodies to T. parva and T. annulata can be detected with an enzyme-linked immunosorbent assay (ELISA), but not commercially available anymore) or an IFA test
• • Serological tests may not be sensitive enough to detect all infected cattle, and cross-reactions can occur with other species of Theileria
• Samples:
• The schizont is the pathogenic stage of T. parva and T. annulata. It initially causes lymphoid proliferation, and later lymphoid destruction. Schizont-parasitised cells may be found in
• • Blood or Buffy coat smears air-dried and fixed in methanol for demonstration of schizonts
• • Lymph node for demonstration of schizonts
• • Impression smears from lung, spleen, kidney and lymph node, air-dried and fixed in methanol, for demonstration of schizonts
• • Lung, kidney, brain, liver, spleen, and lymph nodes for histopathology: demonstration of schizonts and infiltrations of immature lymphocytes
• • A nervous syndrome called ‘turning sickness’ is sometimes observed and intravascular and extra vascular aggregations of schizont-infected lymphocytes are observed, causing thrombosis and ischaemic necrosis throughout the brain
• • Serum for antibody detection
•
• Procedures
• Identification of the agent
• • The presence of multinucleate intracytoplasmic and free schizonts, in lymph node biopsy smears, is a characteristic diagnostic feature of acute infections with T. parva and T. annulata
• • The demonstration of schizont-infected cells in Giemsa-stained blood smears, lymph node impression smears, or histological sections, is diagnostic of ECF
• • Small piroplasms in erythrocytes are suggestive of ECF, but diagnosis must be confirmed by the detection of schizonts
• • Schizonts can be detected in sections but are best seen in smears of lymph node biopsies
• o As there is considerable similarity between schizonts of other theileria parasites
(T. mutans, T. velifera, T. taurotragi and T. buffeli), which may co-infect an animal, it is
important to differentiate the infecting species; this can be done by using serological and
DNA-based assays
• • Piroplasms of most species of Theileria may persist for months or years in recovered animals, and may be detected intermittently in subsequent examinations, however, negative results of microscopic examination of blood films do not exclude latent infection
• • Relapse parasitaemia can be induced with some Theileria species by splenectomy
• • Piroplasms are also seen in prepared smears at post-mortem, but the parasites appear shrunken and their cytoplasm is barely visible
• • A range of probes is available to detect all the Theileria species that are known to infect cattle and are based on 18S ribosomal RNA gene sequences
• • A number of PCR methods (targeting sequences TpR, p104, p67, PIM) can be used to detect
• T. parva and T. annulata
•
• Serological tests
• • The most widely used diagnostic test for Theileria species is the IFA test; both schizont and
piroplasm antigens may be used
• o the IFA test is sensitive, fairly specific, and usually easy to perform
• o because of the problems of cross-reactivity among some Theileria species, the test has
limitations for large-scale surveys in areas where species distribution overlaps
• o the IFA test for T. parva, does not distinguish among the different immunogenic stocks
• • The new indirect ELISAs for T. parva, and T. mutans, based on recombinant parasite-specific
antigens, have demonstrated higher sensitivity and specificity and have largely replaced the IFA
tests previously used in Africa
• • Serological tests based on the ELISAs are being used increasingly for the detection of parasite-
specific antibodies
• • ELISAs have been successfully adapted for the detection of antibodies to T. annulata, and have
been shown to detect antibodies for a longer period of time than the IFA. Indirect ELISAs for
• T. parva and T. mutans have been extensively evaluated in the laboratory and the field, and are now being used in large parts of Africa
• o These tests provide higher (over 95%) sensitivity and specificity than IFA tests but are
not available commercially
•
• PREVENTION AND CONTROL
• Sanitary prophylaxis
• • Bovine theileriosis is generally controlled by the use of acaricides to kill ticks, but this method isnot sustainable
• • Acaricides are expensive, they cause environmental damage, and over time ticks develop resistance to them requiring newer acaricides to be developed
• • More sustainable and reliable methods for the control of theileriosis that deploy a combination of strategic tick control and vaccination are desirable, however, these are yet to be successfully applied on a large scale in endemic areas
• • Sanitation and disinfection measures are not generally effective in preventing transmission of
theileriosis
•
• Medical prophylaxis
•
• • Chemotherapeutic agents such as buparvaquone are available to treat T. parva and T. annulata infections
• • Treatments with these agents do not completely eradicate theilerial infections and lead to the development of carrier states in their hosts
• • Recovery from one strain of T. annulata confers cross-protection against most other strains
• • Complete cross-protection does not occur with T. parva
• Inactivated vaccines
• • None are available
Live attenuated vaccines
• • Reliable vaccines of known efficacy have been developed for T. parva and T. annulata
• • For T. annulata, the vaccine is prepared from schizont-infected cell lines that have been isolated from cattle and attenuated during in-vitro culture
• • The vaccine must remain frozen until shortly before administration
• • Vaccination against T. parva is based on a method of infection and treatment in which cattle are given a subcutaneous dose of tick derived sporozoites and a simultaneous treatment with a long-acting tetracycline formulation
• o This treatment results in a mild or inapparent East Coast fever reaction followed by recovery
• o Recovered animals demonstrate a robust immunity to homologous challenge, which usually lasts for the lifetime of an animal
• • Immunisation of animals with a stock(s) engendering a broad-spectrum immunity is desirable to cover a range of immunological T. parva strains that exist in the field.
• • Immunised animals usually become carriers of the immunising parasite stock(s)
• • Consideration should be given to the risk of introducing new isolates into an area where they may then become established through a carrier state
•
• Recombinant vaccines
• • Experimental subunit vaccines are being developed for ECF, and ideally will contain antigens from both sporozoite (as the p67 protein) and schizont stages. An improved p67 vaccin has been tested in the field and might be available soon
• PUBLIC HEALTH
• There is no evidence that T. parva or T. annulata are hazards to humans.
•
Reference-,On request