Traumatic Reticuloperitonitis[TRP] (Hardware disease, Traumatic gastritis)
Compiled & shared by-DR. Amit Bhardwaj,Large &Small animal surgery specialist,Pune
Traumatic reticuloperitonitis develops as a consequence of perforation of the reticulum. It is important as a differential diagnosis of other diseases marked by stasis of the GI tract, because it causes similar signs. Traumatic reticuloperitonitis is most common in mature dairy cattle, occasionally seen in beef cattle, and rarely reported in other ruminants.
Cattle commonly ingest foreign objects, because they do not discriminate against metal materials in feed and do not completely masticate feed before swallowing. The disease is common when green chop, silage, and hay are made from fields that contain old rusting fences or baling wire, or when pastures are on areas or sites where buildings have recently been constructed, burned, or torn down. The grain ration may also be a source because of accidental addition of metal.
Etiology:
Swallowed metallic objects, such as nails or pieces of wire, fall directly into the reticulum or pass into the rumen and are subsequently carried over the ruminoreticular fold into the cranioventral part of the reticulum by ruminal contractions. The reticulo-omasal orifice is elevated above the floor, which tends to retain heavy objects in the reticulum, and the honeycomb-like reticular mucosa traps sharp objects. Contractions of the reticulum promote penetration of the wall by the foreign object. Compression of the ruminoreticulum by the uterus in late pregnancy and straining during parturition increase the likelihood of an initial penetration of the reticulum and may also disrupt adhesions caused by an earlier penetration.
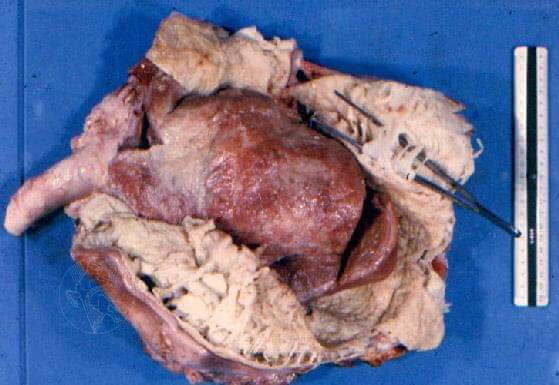
Perforation of the wall of the reticulum allows leakage of ingesta and bacteria, which contaminates the peritoneal cavity. The resulting peritonitis is generally localized and frequently results in adhesions. Less commonly, a more severe diffuse peritonitis develops. The object can penetrate the diaphragm and enter the thoracic cavity (causing pleuritis and sometimes pulmonary abscessation) and the pericardial sac (causing pericarditis, sometimes followed by myocarditis). Occasionally, the liver or spleen may be pierced and become infected, resulting in abscessation, or septicemia can develop.
Clinical Findings:
The initial penetration of the reticulum is characterized by the sudden onset of ruminoreticular atony and a sharp fall in milk production. Fecal output is decreased. The rectal temperature is often mildly increased. The heart rate is normal or slightly increased, and respiration is usually shallow and rapid. Initially, the cow exhibits an arched back; an anxious expression; a reluctance to move; and an uneasy, careful gait. Forced sudden movements as well as defecating, urinating, lying down, getting up, and stepping over barriers may be accompanied by groaning. A grunt may be elicited by applying pressure to the xiphoid or by firmly pinching the withers, which causes extension of the thorax and lower abdomen. The grunt can be detected by placing a stethoscope over the trachea and applying pressure or pinching the withers at the end of an inspiration. Tremor of the triceps and abduction of the elbow may be seen.
In chronic cases, feed intake and fecal output are reduced, and milk production remains low. Signs of cranial abdominal pain become less apparent, and the rectal temperature usually returns to normal as the acute inflammation subsides and peritoneal contamination is walled off. Some cattle develop vagal indigestion syndrome (see Vagal Indigestion Syndrome in Ruminants) because of the adhesions that form after foreign body perforation, particularly those on the ventromedial reticulum.
Cows with pleuritis or pericarditis due to foreign body perforation usually are depressed, tachycardic (>90 bpm), and pyrexic (104°F [40°C]). Pleuritis is manifest by fast, shallow respiration; muffled lung sounds; and possibly pleuritic friction rubs. Thoracentesis may yield several liters of septic fluid. Traumatic pericarditis is most commonly characterized by muffled heart sounds; however, early in the disease process pericardial friction rubs or gas and fluid splashing sounds (washing machine murmur) can be heard on auscultation. Jugular vein distention and congestive heart failure with marked submandibular and brisket edema is a frequent sequela of traumatic reticulopericarditis. Prognosis is grave with these complications. Penetration through the pericardium into the myocardium usually results in extensive hemorrhage into the pericardial sac or ventricular arrhythmias and sudden death.
Diagnosis:
This can be based on history (when available) and clinical findings if the cow is examined when signs initially appear. Without an accurate history and when the condition has been present for several days or longer, diagnosis is more difficult. Other causes of peritonitis, particularly perforated abomasal ulcers, can be difficult to distinguish from traumatic reticuloperitonitis. Differential diagnoses should include conditions that can produce variable or nonspecific GI signs, eg, indigestion, lymphosarcoma, or intestinal obstruction. Abomasal displacement or volvulus should be excluded by simultaneous auscultation and percussion. Pleuritis or pericarditis of nontraumatic origin produces signs similar to those associated with foreign body perforation.
Although not always necessary, laboratory tests may be helpful. In many cases, there is a neutrophilia with a left shift. Plasma fibrinogen concentrations may be increased, and serum haptoglobin, amyloid A, and total plasma protein concentrations may be markedly increased. Severely affected cattle may have coagulation abnormalities, as evidenced by prolonged prothrombin time, thrombin time, and activated partial thromboplastin time. The acid-base status and serum electrolyte levels are typically normal, because abomasal and small-intestinal absorption can remain normal. However, marked hypokalemic, hypochloremic metabolic alkalosis can be seen, presumably because adynamic ileus from peritonitis can affect abomasal and GI motility and resorption of abomasal secretions. The metabolic alkalosis can be created or exacerbated by treatment with alkalinizing agents such as magnesium hydroxide used as a laxative. Peritoneal fluid analysis can help determine whether peritonitis is present, particularly the concentration of D-dimer and the neutrophil percentage in the peritoneal fluid. However, the peritonitis frequently becomes walled off, and in these cases peritoneal fluid may be within the reference range unless obtained from within the lesion. The presence of a magnet in the reticulum can be determined by movement of a magnetic compass in the region of the cranioventral abdomen; the presence of a magnet in the reticulum makes traumatic reticuloperitonitis very unlikely unless the penetrating object is not magnetic.
Ultrasonography of the ventral abdomen using a 3-MHz transducer is the most accurate way to diagnose localized peritonitis near the reticulum and characterize the reticular contraction frequency. It rarely identifies the presence of a penetrating object. Ultrasonography of the heart and thorax is very useful in the diagnosis of pleuritis and pericarditis as a sequelae of traumatic reticuloperitonitis and has replaced radiography in the diagnosis of reticuloperitonitis.
Lateral radiographs of the cranioventral abdomen can detect metallic material in the reticulum but should be taken only after oral administration of a magnet. To determine whether the reticulum is currently perforated, the foreign body must be visible beyond the border of the reticulum, unattached to the magnet in the reticulum, or positioned off the floor of the reticulum. A depression in the cranioventral aspect of the reticulum or identification of an abscess (by gas accumulation outside a viscus), soft-tissue masses, or a fluid line in the cranial abdomen are also reliable radiographic findings of penetration. Portable radiographic units cannot penetrate the reticular area of standing adult cattle, and the cow may need to be transported to where there is equipment with sufficient power. The cow should not be placed in dorsal recumbency to obtain radiographs, because such manipulation places stress on adhesions and may lead to a localized peritonitis becoming a diffuse peritonitis due to gravitational spread of infection.
Electronic metal detectors can identify metal in the reticulum but do not distinguish between perforating and nonperforating foreign bodies.
Treatment:
Treatment of the typical case seen early in its course may be surgical or medical. Either approach improves the chances of recovery from ~60% in untreated cases to 80%–90%. Surgery involves rumenotomy with manual removal of the object(s) from the reticulum; if an abscess is adhered to the reticulum, it should be aspirated (to confirm it is an abscess) and then drained into the reticulum. Antimicrobials should be administered perioperatively. Medical treatment involves administration of antimicrobials to control the peritonitis and a magnet to prevent recurrence. Because of the mixed bacterial flora in the lesion, a broad-spectrum antimicrobial agent such as oxytetracycline (16 mg/kg/day, IV) should be used. Penicillin (22,000 IU/kg, IM, once to twice daily) is widely used and effective in many cases despite its limited spectrum. Affected cows should be confined for 1–2 wk; placing them on an inclined plane (elevated in front) is believed by some to limit further penetration of the foreign object, but supporting studies are lacking. Supportive therapy, such as oral or occasionally IV fluids and SC calcium borogluconate or calcium gluconate, should be administered as needed. Rumen inoculation (4–8 L of ruminal fluid from a healthy donor) is beneficial in some cases with prolonged ruminal stasis and loss of normal flora.
More advanced cases, those with obvious secondary complications, or those that do not respond to initial medical or surgical therapy should be evaluated from an economic perspective; if the cow is of limited value, slaughter should be considered if the carcass is likely to pass inspection.
Laboratory Testing
Complete blood count – The CBC in a cow with TRP can vary depending on whether the peritonitis is acute or chronic and localized or diffuse. In general, cattle with persistent purulent inflammation have leukocyte counts ranging from 4,000-15,000/µL, with neutrophilia. Although lymphocytes are the predominant leukocyte circulating in healthy cattle, endogenous corticosteroid release secondary to stress may cause lymphopenia by cell redistribution; circulating lymphocytes do not re-enter the lymphatics but become sequestered in lymphoid tissue and bone marrow.
Some cattle with acute, localized peritonitis will have CBCs within normal reference intervals, while others will have a degenerative left shift (band neutrophils outnumbering segmented neutrophils). Cattle with acute diffuse peritonitis will also have a degenerative left shift. In chronic cases, a mature neutrophilia is common.1 Neutrophil counts in these individuals are often greater than 4,000/µL. Affected cattle also will show hyperfibrinogenemia, with fibrinogen concentrations greater than 1,000 mg/dL.2Fibrinogen is an acute phase protein, and in cattle it may be the best indicator of acute inflammation because fibrinogen concentrations often increase prior to development of neutrophilia.7
Hematology data can be used to detect inflammation, but generally cannot identify a specific cause of inflammatory disease. Other tests may be useful in differentiating between different inflammatory diseases, such as TRP
Serum biochemical profile – The most common chemistry abnormality associated with TRP is hyperproteinemia with a hyperglobulinemia. Some authors suggest that a total serum protein concentration greater than 10 mg/dL is highly suggestive of TRP.2,5 In one study of cattle suspected of having TRP that also had a total plasma protein concentration of 100 g/L (10mg/dL) had an 83% chance of having TRP, 83% of the cattle with a total plasma protein concentration of 10 mg/dL had TRP.
Other chemistry abnormalities associated with TRP may include hypochloremia, hypokalemia, and metabolic alkalosis; these abnormalities occur secondary to ruminal hypomotility and/or vagal indigestion. Hypochloremic metabolic alkalosis may occur due to sequestration of hydrochloric acid in the rumen caused by rumen stasis or vagal indigestion. Hypokalemia is caused primarily by anorexia, but may be potentiated slightly by ion exchange caused by the alkalosis and/or abomasal reflux into the rumen. With alkalosis, intracellular H+ ions can be exchanged for extracellular K+ ions, decreasing serum potassium concentrations. This effect is minor compared to the K+ ion shifts associated with acidosis.
Abdominocentesis – Normal peritoneal fluid of an adult cow is straw-colored, clear, and odorless. Protein and fibrinogen concentrations can vary from 1.0-3.0 g/dL and 100-500 g/dL, respectively. The nucleated cell count should be less than 10,000 cells/µL. The majority of nucleated cells are non-degenerate neutrophils and mononuclear cells. At least 10% of the nucleated cell population should consist of eosinophils.3 Turbid samples or samples containing gross pus or fibrin are indicative of peritonitis, at least locally. It is, however, normal for bovine peritoneal fluid to clot upon standing. Nucleated cell count, cell percentages, and character of cells present can be suggestive of disease. If a sample contains immature, degenerative (Fig. 5), or toxic neutrophils (especially if the NCC is greater than 10,000 cells), purulent peritonitis is present. Purulent peritonitis is indicated by an abdominal fluid sample with greater than 40% neutrophils. The presence of intracellular bacteria and/or degenerate neutrophils indicates septic peritonitis.
Figure 5. Two degenerative neutrophils with phagocytosed bacteria in abdominocentesis fluid from a cow with traumatic reticuloperitonitis (hardware disease). Bacteria also are scattered in the background of the smear (Wright stain).
Normal cytologic findings do not exclude TRP since cattle tend to wall off inflammation in the peritoneal cavity, making it more difficult to diagnose local peritonitis. Abdominocentesis for evaluation of TRP should be performed at the ruminal-reticular recess to increase the chance of obtaining a diagnostic sample.3 The reference ranges for calves vary significantly from adult cattle. The most notable difference between normal peritoneal samples in calves versus adult cattle is the protein concentration and percentages of neutrophils and eosinophils. Adult ranges should not be used to evaluate peritoneal fluid obtained from younger animals.
Differential Diagnoses
TRP must be distinguished from other causes of peritonitis or abdominal pain for a definitive diagnosis. In febrile animals, the most likely differential diagnosis is a perforating abomasal ulcer. A perforating abomasal ulcer can be distinguished from chronic TRP since a cow with chronic TRP is typically afebrile and has cranial ventral abdominal pain, whereas a cow with a perforating abomasal ulcer typically has mid-abdominal pain.1 Also, cattle with a perforating abomasal ulcer may show evidence of gastrointestinal leakage, such as plant material, on abdominocentesis, microorganisms, and/or squamous cells in the abdominal fluid. The most likely differential diagnoses for an afebrile animal are indigestion and ketosis. Cows with indigestion or ketosis should not be painful and ketotic cows will have ketones in their urine, as detected by dipstick analysis.1Overall, the best differentiator of these diseases is total plasma protein levels. Total plasma protein should not be increased in a cow with either indigestion or ketosis and are less severely increased in a cow with a perforating abomasal ulcer.
Complications of TRP
Reticular abscesses are a common complication of TRP. Also, if the foreign body migrates through the diaphragm and into the pericardium, it can cause septic pericarditis and subsequent congestive heart failure. Less common complications include reticular fistulation, vagal indigestion, and diaphragmatic hernia.
Prevention:
Preventive measures include avoiding the use of baling wire, passing feed over magnets to remove metallic objects, keeping cattle away from sites of new construction, and completely removing old buildings and fences. Additionally, bar magnets may be administered PO, preferably after fasting for 18–24 hr. Usually, the magnet remains in the reticulum and holds any ferromagnetic objects on its surface. There is good evidence that giving magnets to all herd replacement heifers and bulls at ~1 yr of age minimizes the incidence of traumatic reticuloperitonitis.
https://basu.org.in/wp-content/uploads/2020/10/TRP.pptx
TRAUMATIC RETICULOPERITONITIS (TRP OR HARDWARE DISEASE) IN DAIRY CATTLE-DIAGNOSIS & TREATMENT
Reference:on request.