TREATMENT OF SNAKEBITE CASES IN CATTLE IN INDIA
Dr.Amit Bhardwaj, Veterinary Surgeon, Pune.
Snake bite cases to livestock are generally considered an emergency cases & it is very challenging task to handle such cases at field level in rural India where the basic infrastructure are lacking.
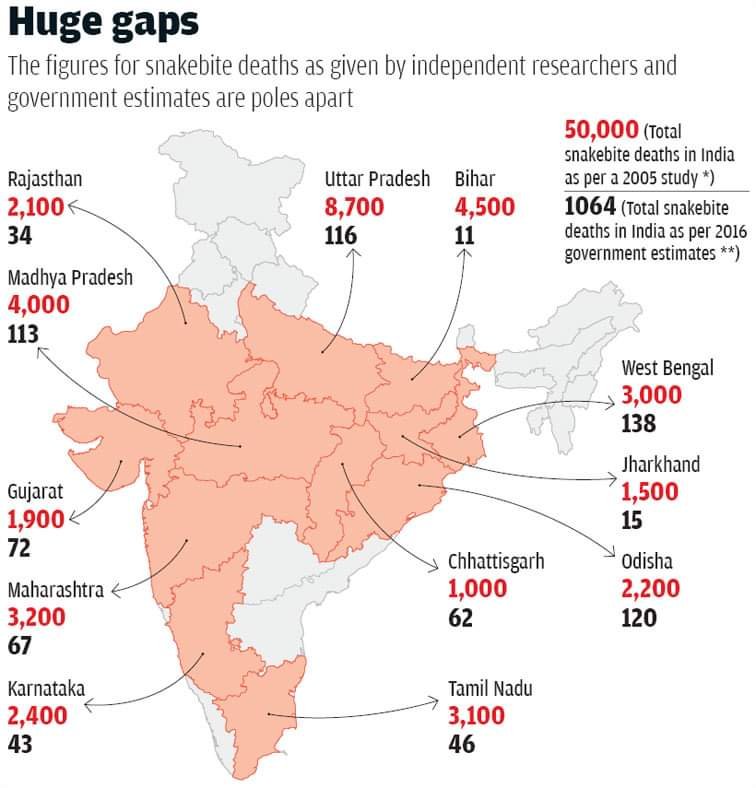
A large percentage of India’s population resides in rural areas and is mostly dependent on agriculture where livestock production dominates . Farmers in rural areas are sometimes faced with livestock diseases and problems like snakebite. There are nearly 216 species of snakes in India in which 60 are considered poisonous. The most poisonous, medically important species of India distributed widely throughout the country, nearly one lakh animals in the world fall prey to venomous snake bite every year. In India Madhya Pradesh has recorded the highest number of snake bite followed by Maharashtra. Snake bites are common in most rural areas and particularly in forest and forest fringe villages. Snake bite in animals generally occurs during grazing or hunting or while playing in the garden. Most of the cases of snake bite have been reported in dogs and horses . The clinical effects are more severe in small animals as compared to large animals. Dogs and cats are most often bitten around the head and limbs.Venom is two type neurotoxic or haemotoxic. Neurotoxic signs are flaccid paralysis, respiratory paralysis. In case of haemotoxic venom, the toxins are released in the blood and cause Arterial thrombosis and necrosis. Snake bite in human and animal that requires rapid examination and critical care for proper treatment.
Cattle are believed to be more vulnerable to snakebite than goats . Snakebite can be a serious problem to cattle in summer and rainy moist seasons when it is warm and favourable for snakes to be out of their holes hunting on pastures where cattle graze. During grazing, cattle are at a high risk of coming in contact with snakes. Snakebite has been reported as a serious problem for livestock all over the world . Documentation of mortalities caused by snakebite in India is scarce. Poisoning by snakebite requires an immediate medical attention. Some farmers are either resource poor or stay far away from urban areas and they cannot easily acquire modern medicine for their livestock. Such farmers usually tend to use traditional remedies. The use of traditional medicine to treat and manage snakebite has been reported in both human beings and livestock in India.
Snake bite in animals generally occurs during grazing or hunting or while playing in the garden. Most of the cases of snake bite have been reported in dogs and horses (Garg, 2000). Poisoning from snake venom in animals is an emergency which requires immediate attention or otherwise delayed and inadequate treatment may lead to untoward consequences.
Many snake bites can cause injury or death in livestock, and treatment depends on the type of animal bitten and its sensitivity to that particular snake’s venom. Horses are at the top of the sensitivity list, followed by sheep, cows, goats, dogs (and humans), pigs and cats.
In year 2017 , the World Health Organization (WHO) included snakebite into the list of “Neglected Tropical Diseases” (NTDs) —a diverse group of tropical infections affecting poor communities in Africa, Asia and the Americas. Activists hope the decision will bring attention to snakebite, so far neglected by pharma firms and policy makers.
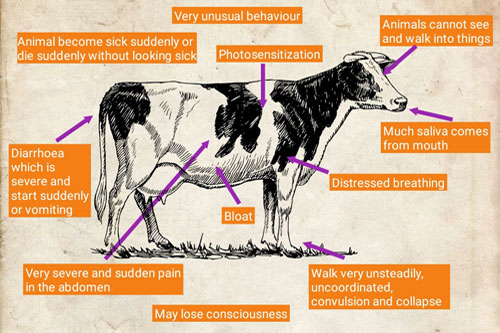
How to identify snake bites
When a sheep is bitten by a poisonous snake, the animal will experience difficulty swallowing, the tongue will protrude limply from the mouth and the animal will dribble saliva.
This may be followed by the expulsion of the stomach contents through the nostrils and the sheep lying down, unable to move. Death can occur as a result of respiratory failure, if bitten by a cobra, or the animal could drown in its own saliva.
For goats, symptoms are similar to those of sheep, though goats show less sensitivity to snake venom. However, goats can die from puff adder bites. Surprisingly little research has been done on snake bites in cattle.
However, although the animals are extremely sensitive to venom, it would appear that death occurs only with multiple bites. Other factors that come into play include the amount of venom injected; the size of both the cow and the snake; and the age and health of the animal.
A healthy cow is less likely to succumb to the effects of venom than an older individual in poor health. Where it was bitten is also important.
Typically, bites occur on the head, face and muzzle area while the animal is grazing, and are far more serious than bites on the legs. Cattle that have been bitten often show signs of a “goose stepping” type of leg action.
Bite types
Venomous snakes fall into two categories: elapids, which include cobras and mambas, and vipers, such as puff adders. Elapids have short fangs and tend to “chew” their venom into their victim.
The poison affects the nervous system and kills by paralysing the respiratory system.
Vipers have long, hinged hypodermic needle-like fangs that penetrate the flesh, delivering venom deep into the tissue. This causes enormous damage to blood vessels and loss of tissue.
Localised bleeding and tissue necrosis can occur even in animals which make a full recovery. In some cases, persistent lameness may occur.
However, many snake bites in livestock are thought to be “dry bites”, where no venom is injected. A snake can determine the size of an animal and its venom is a valuable resource it doesn’t waste indiscriminately.
Therefore a dry bite is delivered as a warning. It’s also important to remember that not all snakes are venomous. Unless you can positively identify the snake, assume that it has delivered a dry bite if no symptoms materialise.
Unfortunately, every year thousands of harmless snakes are killed, when, in fact, they are one of the best rodent predators a farmer could wish for.
DIAGNOSIS
On the basis of history and physical examination of the animal is suspected for snakebite. The clinical parameters like rectal temperature, pulse and respiratory rate are increased. The blood sample collected from the said animal with ethylene diamine tetra acetic acid (EDTA) for hematological parameters like haemoglobin, packed cell volume and total leukocyte count estimation. The hematological parameters reveal the decreased hemoglobin concentration and packed cell volume and increased total leukocyte count are seen in the animal.
TREATMENT
The animals are treated in the snakebite case depending upon condition & severity but an standard line of treatment is like this—
The animal is treated with polyvalent snake venom anti- Serum (Bharat Serums &Vaccines Limited ,Thane – India).snake venom antiserum along with 500 ml of 5% dextrose are administered intravenously followed by Dexamethasone at the dose of 2mg/kg is administered and Atropine Sulphate at the rate of 0.04mg/kg intramuscularly. Chlorpheniramine malate 10 ml and Botrophase 10ml are also given intravenously. In addition, Enrofloxacin at the dose of 5 mg/kg, i/m and tetanus toxoid (serum institute of India) 2ml i/m are also given. The antibiotic therapy is continued for 5 days to the said animal along with and liver tonic.
NB——-
Snake venom is a highly complex cocktail of proteins, peptides, non-protein toxins, carbohydrates, lipids, amines and other molecules. The chemical composition of venom varies at all taxonomic levels. The snake venom mainly contains proteins (>90%, dry weight). There are more than hundred different proteins in each venom; with elapid and viperid venoms constituting 25-70% and 80-90% of enzymes respectively. Some non-enzymatic polypeptide toxins and non-toxic proteins are also present .The snake venoms are mainly characterized as neurotoxic and hemotoxic. The neurotoxic venoms act at molecular level, by disrupting the neuromuscular junctions, limiting muscle activity while hemotoxic venoms cause tissue destruction in body systems besides their effect on circulatory system.The venom enzymes include hydrolases, hyaluronidase, kininogenase. Other enzymes include phosphomono-and diesterases,5’- nucleotidase, DNAase, NAD-nucleosidase, l-amino acid oxidase, phospholipase A2(PLA2), peptidases and zinc metalloproteinase hemorrhagins. Hyaluronidaseaids in venom dissemination from the bite site through tissues .The toxins such as the haemorrhagins cause spontaneous bleeding in the gingival sulci, nose, skinand gastrointestinal tract . The most effective antidote against snake venom is the anti-snake venom. It is usually pepsin refined F (ab) fragments of IgG purified from the serum or plasma of a horse or sheep that has been immunized with the venom of one or more species of snakes. ASV neutralizes the venom of a particular species (monovalent/ monospecific) or various different species (polyvalent/polyspecific). The antibodies against a particular species may also neutralize thevenom of a closely related species (Para specific activity). In India, horses are hyper immunized against the venom of four common poisonous snakes the “Big Four” (Cobra, Krait, Russell’s viper and Saw-scaled viper), to produce polyvalent anti snake venom. Sometimes lyophilized polyvalent anti-snakevenom may cause anaphylactic reactions to overcome the untoward effect to antivenom;dexamethasone injection is given to the animal. However, some study tells corticosteroid is preferred over antihistamines as in certain times it potentiates the toxic action of the snake venom . Prophylactically, Tetanus toxoid and broad spectrum antibiotic is administered to the animals ; asthe fangs of the snake are supposed to be contaminated with various types of bacteria Treatment usually consists of intravenous fluids and the administration of antivenom to neutralize the snake venom in the animal’s body.
First aid
Before calling the vet, try and determine if the animal has actually been bitten by a venomous snake. Although it may be difficult to locate the bite due to the hair on the animal’s body, bleeding or swelling are good signs to look out for.
A bite from a venomous snake will leave two quite distinctive puncture wounds, which will bleed profusely in the case of a puff adder bite.
A bite from a non-venomous snake will probably leave no teeth marks, unless it was from a large python. Teeth marks result in multiple puncture wounds and copious bleeding.
Some tips
• If the animal has been bitten in the nostrils or muzzle, these areas will swell, making it difficult for the animal to breathe. Pass a piece of clean tubing up the nostrils to maintain an open airway. Where the animal shows signs of paralysis, breathing down the tube will help keep it alive until the vet arrives.
• Keep the animal calm, as an increased heart rate will spread venom through the body much more rapidly. Let the vet come to the animal rather than trying to walk it to a more accessible spot, as this will only increase its heart rate.
• Never cut the wound and try to suck out the venom. If you have a cut in your mouth, you’ll be poisoned as well.
• In the case of a cobra bite (excluding the Mozambique spitting cobra), apply a pressure bandage over the bite and wrap it up to the top of the limb. This is not a tourniquet as its aim isn’t to stop blood flow, but to slow down the venom’s absorption into the lymph system. (If applied to a viper bite, where swelling develops, this will do more harm than good.)
• For viper and spitting cobra bites, simply keep the animal calm, and seek veterinary treatment as quickly as possible.
• Do not apply a hot or cold compress, as this could damage the tissue even further.
• Do not administer any form of alternative treatment. The only proven treatment for snake bites is anti-venom.
• Your vet should be able to determine whether the animal was bitten by a snake, whether or not venom was injected, what type of snake it was and if the animal requires anti-venom. Some animals may recover simply with supportive care.
PREVENTION OF SNAKE BITE CASES IN INDIA
Prevention of this acute, life-threatening medical emergency is the mother of cure. At the household level, measures include eradication of rats; avoiding having rubble, firewood, and cattle sheds in residential areas; wearing of high-sided footwear; use of a torch and stick while walking during darkness on farms and in high-grown grass; sleeping on a bamboo cot with the edges of a mosquito net properly tucked under the bed; and strict prohibition of open toileting. Villagers need to be trained to identify venomous snakes and on how to prevent bites. Additionally, strict police action should be taken against mantriks and ojhas (village healers).
After a snake bite, rather than wasting time by attending a mantrik or using herbal remedies, patients with a bitten part below the heart level should be immediately transferred to a qualified vet.
Governments should make it compulsory that vets should be given proper training on the identification of venomous snakes (should patients bring the killed specimen), on early diagnosis of clinical manifestations, and on the correct dose of ASV.
Additionally, many vet officers are afraid of anaphylactic reactions to ASV. Anaphylaxis can be prevented by administering subcutaneous epinephrine before ASV, or easily reversed by intramuscular epinephrine, intravenous fluids, steroids, antihistamines, and temporary termination of the ASV drip .The production of ASV requires milking of venom and use of horses for antivenin. The time is right to alleviate snakebite mortality and morbidity due to snakebite envenoming in cattle in south Asia.
REFERENCE:On request
Photo: Courtesy , Google.