TRICHURIASIS OR WHIPWORM INFECTION IN ANIMALS
Trichuris is a widespread gastrointestinal parasite that can be found in a broad range of hosts and causes trichuriasis, a neglected tropical disease causing significant animal and human health problems as well as considerable socio-economic consequences worldwide . Among the various species of Trichuris, Trichuris ovis is a whipworm infecting the caecum and colon of sheep, goats, cattle and other ruminants in all parts of the world. Its life cycle is direct where definitive host acquired infection through ingestion of infective stage of L1 within the eggs which hatch in the small intestine and the released larvae burrow into the intestinal wall of the caecum and proximal colon where they develop to mature worms.
Morphology
The male measures 50-80 mm in length of which the narrow and filamentous anterior end constitutes three-quarters of the length . The female is 37- 70 mm long of which the narrow and filamentous anterior end forms two-thirds to four-fifths . The fully evaginated spicule is 5-6 mm long and having a sheath which bears an oblong swelling a short distance from its distal extremity and is covered with minute spines which decrease in size towards the distal extremity . The characteristics eggs are brown, barrel shaped or lemon shaped with a transparent, conspicuous plugs at both ends and measures 70-80 by 30-42mm including the plugs; they contain an unsegmented embryo when laid .
Life cycle
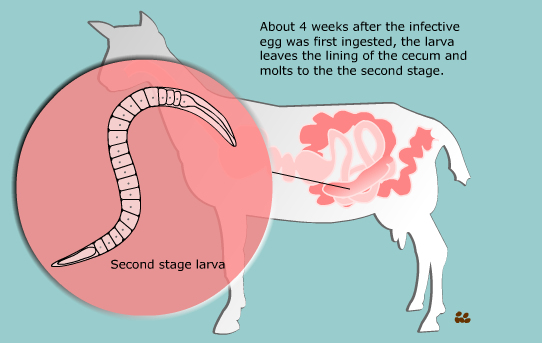
Its life cycle is direct where orally ingested embryonated eggs hatch in the small intestine and the released larvae burrow into the intestinal wall of the caecum and proximal colon where they develop to mature worms. The anterior end of the worm forms syncytial tunnels of epithelial cells around itself as it burrows through the mucosa . The posterior end protrudes into the lumen facilitating copulation and egg release. The infective stage is L1 within the egg which develops in three weeks under favourable conditions . Infective stage develops in one or two months of being passed in the faeces depending on the temperatures (e.g. 6-20 °C), since development is related to soil moisture and temperature . Under optimal conditions these may subsequently survive for several years . After ingestion, the plugs are digested and the released L1 penetrate the glands of the anterior small intestine for 2 to 10 days before they move to caecal mucosa, where they develop to adults . Subsequently all four moults occur within these glands, the adult emerging to lie on the mucosal surface with their anterior ends embedded in the mucosa. The prepatent period is 7-9 weeks .
Pathogenesis
The filamentous narrow anterior end of T. ovis may be embedded in mucosa, surrounded with fibroblast and leucocytes without sign of fibrosis and necrosis . T. ovis inserted in the lining of the large intestine predominantly in caecum of the hosts may be found exclusively beneath the mucosal layer covered by the apical surface of mucosal epithelium, forming a tunnel. The crypts of Leiberkuhn, submucosa, muscularis mucosae and muscularis externa may be obviously distinguished with slight infiltration of mononuclear cells leucocytes, goblet cells along with epithelial changes and overall mucosal architecture in vicinity of worm penetration . Leucocyte infiltration around the worm embedded under the mucosa but there is no sign of rigid encapsulation, fibrosis, and necrosis . This is probably due to the reason that the penetration of anterior end to receive its nutrition is a normal phenomenon and parasite move to new location after a brief period. But since the penetration of parasite inflame the tissues, leucocytes invasion takes place in the vicinity of the parasite in the inflamed areas . Goat infected with T. ovis show active hyperaemia, haemorrhages and lymphocytic infiltrations in the mucosa . The animal gets infection through ingestion of infective larval stage within the eggs. After ingestion eggs are hatched out to L1, the larvae penetrate into small intestine’s mucosa and stayed for about two weeks which probably provoke desquamation of the epithelium, hyperaemia, mucoid dystrophy, eosinophilic infiltration around the larvae . The larvae and mature worm also induce mechanical damage to the mucosa of small and large intestines followed by extensive local inflammation and haemorrhages. As the parasitic infection is a long standing encroachment on the intestinal wall, especially in untreated animals, it causes destruction of the lining epithelium where they predominantly inhabit. Due to this continuous irritation of the adult parasites on the intestinal wall, catarrhal inflammation occurs. That is why goblet cells were increased in numbers and size .
Clinical signs
A high incidence of light infections with negligible clinical signs is characteristic feature of Trichuris infection in ruminants but isolated outbreaks have been recorded . Most of the infections caused by T. ovis are generally light and asymptomatic . In some cases a large number of worms cause a diphtheritic inflammation of the caecal mucosa. They cause mild to moderate degree of damage in the intestinal surface, resulting in petechial haemorrhages during the process of penetration of the anterior part of the T. ovis . If the host is heavily infected, a large portion of the blood vessels located in the caecal wall will be consumed. This eventually results in the thickening of the wall, thus preventing that region of the large intestine from absorbing fluids causing the host to have diarrhoea Lambs with heavy infection may suffer from bloody colitis and diphtheritic caecitis due to ulcerative and necrotic lesions on the mucosa. Moreover, in animals with high worm burden severe anaemia and dehydration and jaundice may lead to the death of the animals .
Post-mortem examination
Infection of Trichuris in large intestine caused thickening of mucosa, lymphoid nodules on the lamina propria is enlarged from which the parasite may produce some chemical mediators that cause lymphoid proliferation locally . Grossly, congestion, haemorrhagic spots, ulcer formation and nodule formation with thickening of the caecal valve may be observed in large intestine.
Treatment
The following anthelmintics can be used in sheep and cattle
1. Methyridine (200 mg/kg) given orally or subcutaneously is highly effective
2. Fenbendazole (5-20mg/kg) is effective.
3. Oxfendazole (2.5mg/kg) is effective against adult parasites (89-99% efficacy) and immature parasites (62- 100% efficacy).
Whipworm Infection in Dogs and Cats
This worm is one of the “big four” intestinal parasites with which our canine friends must often contend: roundworms, tapeworms, hookworms, and whipworms. The whipworm that affects dogs (Trichuris vulpis) is substantially smaller than the other worms (a mere 30-50 mm in length, about two inches maximum) and is rarely seen as it lives in the cecum (the part of the large intestine where the small and large intestine meet). The head (or, more accurately, the digestive end of the worm) is skinny versus its stout tail (or reproductive end), which gives the worm a whip shape, hence the name.
In the host’s digestive tract, food passes from the mouth to the esophagus to the stomach to the small intestine to the large intestine to the rectum, and then to the outside world. This means the large intestine is one of the last stops for nutrients, and by this point in the journey, nutrients have largely been broken down and absorbed. The large intestine, also called the colon, serves to absorb water, store fecal material, and provide a home for a spectacular number of bacteria that are able to digest leftover food. The large intestine is the home of the whipworm. The adult worms bite the tissue of the intestine, actually embedding their heads inside, and suck blood there.
Eggs are laid inside the large intestine and pass with the stool. Once in the outside world, the eggs require about two-to-four weeks to form embryos and become capable of infecting a new host. (This means that contaminated soil is the source of infection, not fresh feces.)
The new host is infected by consuming the egg, usually during grooming. The egg hatches in the small intestine, releasing a larva. The larva dives into the local glandular tissue and, after about a week, emerges into the small intestine and is carried downstream into the large intestine with the digested food. Once in the cecum or large intestine, its permanent home, it embeds in the tissue there, and after a total of 74 to 87 days from the time the egg was swallowed, the young whipworm is ready to mate.
Signs of Infection
A few whipworms generally do not pose a problem for the host, but if large numbers of worms are embedding themselves in the large intestine tissue, tremendous inflammation can result, leading to bloody, gooey diarrhea. Usually, there is not enough blood loss to be dangerous, but diarrhea readily becomes chronic and hard to control. A second syndrome of infection has emerged but is not well understood: signs mimicking those of Addison’s disease (hypoadrenocorticism). Here, waxing and waning weakness with the inability to conserve salt ultimately creates a dehydration crisis. The syndrome mimics Addison’s disease in every way except that testing for Addison’s disease will be negative and deworming yields a complete recovery.
Because female whipworms only periodically lay eggs (whereas other female worms lay eggs continuously), a fecal sample tested may easily be negative for eggs. This makes confirmation of a whipworm infection a challenge. It is common to deworm whipworms if the symptoms are suggestive of their presence, even if the fecal test is negative. Most common deworming agents do not work on whipworms, so something special must be selected. The most common products are fenbendazole (Panacur®), and febantel (Drontal Plus®).
Thanks to the long maturation cycle of young worms, a second deworming some 75 days or so after the first deworming is needed to fully clear the infection (easy to forget). Often another deworming in between these doses is recommended to further control the whipworm numbers.
Products Effective against Whipworms
More recently, regular heartworm prevention products have been developed to remove and control whipworms: Milbemycin-based heartworm preventives (such as Sentinel®, Interceptor®, and Trifexis®) will cover whipworms, and their regular use covers the second deworming as well. Advantage Multi®, which is a moxidectin-based heartworm preventive, will also cover whipworms.
Soil contaminated by whipworm eggs is contaminated for years. It is virtually impossible to remove the eggs from the soil or kill them. This potential for environmental contamination is concerning, but while there are scattered reports in the medical literature supporting human infection, the Companion Animal Parasite Council does not consider the canine whipworm to be transmissible to humans until there is stronger evidence.
Feline Whipworm Infection
There are species of whipworms that can infect cats: Trichuris serrata in North America and Trichuris campanula in Europe. Cats are clean animals and fastidious around feces, and they rarely get infected. When they do, worm numbers are so small that symptoms hardly ever occur. Whipworms are more of an interesting incidental finding in cats when whipworm eggs happen to come up on a routine fecal check. In other words, feline whipworm infection is generally not considered to be much of a problem.
Compiled & Shared by- Team, LITD (Livestock Institute of Training & Development)
Image-Courtesy-Google
Reference-On Request.
TRICHURIASIS IN SHEEP AND GOAT