TULAREMIA AS AN INFECTIOUS DISEASE & BIOLOGICAL WEAPON THREAT
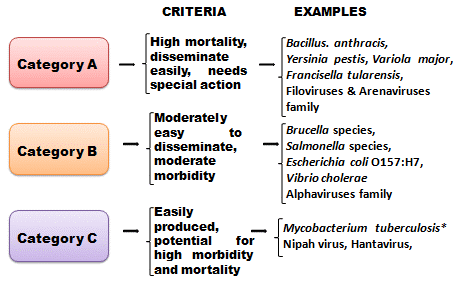
A bioweapon is a virus, protozoan, bacterium, parasite, or fungus that can purposefully be turned into a weapon and deployed against fellow humans during war. Self-replicating toxins and pathogens can also be turned into bioweapons with devastating effects. To date, there exist an estimated 1,200 different kinds of bioagents that have already been weaponized or possess the potential to be turned into a bioweapon. More than 500 million people have died of infectious diseases in the past century, and most have been attributed to bioweapons. The first time pathogens and toxins were deployed in the war was 1763 when the British Army used smallpox against the Native American Indians during the French and Indian war. Another occasion popped up during WWI when Germany attacked its enemies with biological weapons. The impact was not that great, but the act alone laid the groundwork for future use of bioweapons. Categories of Bioweapons:
Here are the most dangerous Bioweapons ever created by humans:
Tularemia
Caused by the Francisellatularensis bacterium, tularemia is another hazardous bio-weapon agent that has a wide range of effects on the human body like skin ulcers, cough, fever, diarrhoea, and vomiting. Infection occurs when humans come into contact with animals infected or killed by tularemia. Being bitten by an infected animal is another sure way of being affected by the disease. During the battle for Stalingrad in WWII, the then Soviet Army is believed to have deployed tularemia against the German forces. Francisellatularensis bacteria is a Category A threat.
Naturally occurring tularemia is a zoonotic disease caused by the bacterium Francisella tularensis, which is a hardy organism capable of surviving for weeks at low temperatures in water, moist soil, hay, straw, or decaying animal carcasses.
There are 4 subspecies of F. tularensis: F. tularensis subsp. tularensis (Type A), which is the most common type in North America, and is highly virulent in humans and animals. F. tularensis subsp. Holarctica (Type B), a less virulent type, responsible for human tularemia infection in Europe and Asia as well as North America; F. tularensis subsp. novocida, another less virulent type; and F. tularensis subsp. mediaasiatica, which is also of low virulence.
Small mammals such as voles, mice, squirrels, and rabbits are natural reservoirs for F. tularensis. These animals acquire tularemia through bites from ticks, fleas, and mosquitoes and also through contact with contaminated environments. Naturally acquired human infection can occur through bites from infected arthropods (usually ticks); contact with infected animal tissues or fluids; direct contact with or ingestion of contaminated water, food, or soil; or inhalation of aerosolized bacteria. Naturally acquired human infection tends to occur predominately in rural areas. F. tularensis is so infectious that simply opening a laboratory culture plate without adequate protective equipment can lead to infection.
Tularemia as a Biological Weapon
tularensisis considered to be a serious potential bioterrorist threat because it is one of the most infectious pathogenic bacteria known-inhalation of as few as 10 organisms can cause disease-and it has substantial capacity to cause serious illness and death. The bacterium was developed into an aerosol biological weapon by several countries in the past.
Aerosol dissemination of F. tularensis in a populated area would be expected to result in the abrupt onset of large numbers of cases of acute, nonspecific respiratory febrile illness beginning 3 to 5 days later.
A World Health Organization (WHO) expert committee reported in 1970 that if 50 kg (110 pounds) of virulent F. tularensis were dispersed as an aerosol over a metropolitan area with a population of 5 million, there would be an estimated 250,000 incapacitating casualties, including 19,000 deaths.
Transmission
Human-to-human transmission is not known to occur.
Infection Control Measures
Since tularemia is not spread from person to person, it is not necessary to place patients diagnosed with tularemia in isolation.
Illness
Symptoms of tularemia depend on the virulence of the bacterial strain and route of infection. Symptoms of all forms of tularemia typically include fever, headache, body aches, and malaise. Symptoms usually develop within 3 to 5 days of infection; however, the incubation period can be 1 to 14 days. Naturally occurring tularemia infection can take several forms, as outlined in the table below. Pneumonic tularemia (the form expected from an aerosol release) is likely to cause typical symptoms of pneumonia (eg, fever, cough, and shortness of breath). Definitive diagnosis requires confirmation by laboratory testing.
| Tularemia: Forms, Routes of Infection, and Symptoms | ||
| Form | Typical route of infection | Symptoms |
| Ulceroglandular | Handling contaminated carcasses or a bite from an infected arthropod | Formation of an ulcer at the site of infection followed by swollen and painful regional lymph glands |
| Glandular | Handling contaminated carcasses or a bite from an infected arthropod | Swollen and painful lymph glands without the development of ulcers |
| Oculoglandular | Direct contamination of the eye with F. tularensis | Pain, redness, swelling, and discharge of the eyes; development of an ulcer on the inside of the eyelid in some cases |
| Oropharyngeal | Eating or drinking contaminated food or water; inhaling aerosolized F. tularensis | Sore throat or tonsillitis; vomiting and diarrhea; possible swelling of the glands in the neck |
| Pneumonic | Inhaling aerosolized F. tularensis; or secondary spread to lungs from another site of infection | Sore throat and swelling of the lymph nodes in the lungs; sudden fever, chills, headache, muscle aches, joint pain, dry cough, and progressive weakness |
| Typhoidal | Unspecified | Systemic illness (fever, chills, headache, etc.) without indication of site of infection or localized symptoms |
| Septic | Unspecified | Potentially severe and fatal; systemic illness (fever, chills, headache, etc.)
Patient typically appears toxic; may develop confusion and coma Without prompt treatment, may lead to septic shock, acute respiratory distress syndrome, and organ failure |
Clinicians who suspect tularemia should promptly obtain blood and other cultures, as appropriate, and alert the laboratory to the need for special diagnostic and safety procedures. F. tularensis may be identified through direct examination of secretions, exudates, or biopsy specimens using Gram stain, direct fluorescent antibody, or immunohistochemical stains. It can be grown from pharyngeal washings, sputum specimens, and even fasting gastric aspirates in a high proportion of patients with inhalational tularemia. It is only occasionally isolated from blood. Rapid diagnostic tests are not widely available; ancillary confirmatory testing via microscopic demonstration of F. tularensisusing fluorescent-labeled antibodies is a rapid diagnostic procedure performed in designated reference laboratories in the National Public Health Laboratory Network. Test results can be available within several hours if the laboratory is alerted and prepared. Growth of F. tularensis in culture is the definitive means of confirming the diagnosis and usually takes 24 to 48 hours in ideal conditions. However, in some instances, growth of the bacteria can be delayed up to 10 days.
The overall case fatality rate for untreated infections with Type A strains has been 5% to 15%, but in pneumonic or septic cases, without antibiotic treatment, the fatality rate has been as high as 30% to 60%. With treatment, the most recent fatality rates in the US have been 2%.
Prophylaxis and Treatment
Early antibiotic therapy is recommended for persons exposed to or infected with tularemia. Tetracyclines (eg, doxycycline), fluoroquinolones (eg, ciprofloxacin), and aminoglycosides (eg, streptomycin and gentamicin) are all effective treatments and doxycycline or a fluroquinolone can be used for prophylaxis after high risk exposure. Following a biological attack, treatment recommendations would depend on antibiotic susceptibility of the strain of bacteria used in the attack.
Since person-to-person transmission is not known to occur, post-exposure prophylaxis of close contacts with persons infected with tularemia is unnecessary.
Countermeasures
In the US, a live-attenuated vaccine derived from the avirulent live vaccine strain (LVS) developed by the Department of Defense (DoD) was used to protect laboratory personnel routinely working with F. tularensis and military high-risk personnel. The vaccine does not provide a high degree of protection from inhalational infection and is not currently in use.
Anthrax
The Bacillus anthracis bacterium is one of the deadliest agents ever to be weaponized in history. The American disease control arms of the government have categorized Bacillus anthracis as a Category A threat, a rank designated for dangerous elements that pose a hazard to national security. The spores that house Anthrax bacteria are naturally present in soils and can also be cultured in a laboratory. What makes them dangerous is their ability to spread quickly and survive for a long time even when exposed to harsh environmental conditions. Anthrax has been used for long as a weapon and was usually mixed with powder, water, and food. In 2001, letters containing powdered anthrax were sent to 22 people across the US, and five of these people later died. The Japanese army deliberately infected Chinese prisoners in Manchuria with anthrax which led to the death of 10,000 people during the WWI. The UK military tested a spore delivery system for anthrax on the island of Gruinard in Scotland, and these pores ended up surviving for a long time affecting people living close to the area.
Botulinum Toxin
Botulinum is a toxin that is relatively easy to produce and can be distributed through aerosols, water contamination and food provisions. The Botulinum toxin is so hazardous that a mere gram of it is potent enough to wipe out a million people when they inhale. Botulinum paralyzes muscles and blurs vision. The bacterium behind Botulinum is called Clostridium. The toxin is naturally present in damp forest soils, lake beds, and shallow streams. Records show that the Japanese army experimented with prisoners in Manchuria by injecting them with Clostridium botulinum leading to grave consequences.
Smallpox
Variola major is a virus responsible for causing smallpox. It is a highly infectious disease with no known treatment, and if it were not for the discovery of its vaccine, it was well on its way to wiping out humans off the face of the planet. Over 300 million humans died of smallpox in the twentieth century, the highest death toll by a disease ever recorded. The weaponization of smallpox was first attempted during the war against Native Americans by the British Army. In 1980, the then Soviet government started a program of developing the smallpox virus for use as a weapon at the height of the cold war. However, smallpox poses no threat of ever being weaponized thanks to the move by the World Health Organization in 1967 to launch a global immunization program.
Ebola
The deadly disease is caused by the Ebola virus, which was first brought to the world’s attention in 1976 when it was encountered in DRC. Transmission is through contact and has a fatality rate of 50%. Between 1986 and 1990, the Soviet Union started a program aimed at weaponizing Ebola. Evidence of that program ever coming to fruition or Ebola being used as a weapon anywhere on earth has never been found. Weaponizing Ebola is possible, but it is a costly endeavour since the disease mainly spreads through contact.
Pneumonic Plague
The plague is caused by a bacterium, Yersinia pestis, which is another Category A organism. The plague carries the most significant potential of being weaponized as it is easy to mass-produce it in a laboratory with minimal cost. It is also one of the oldest bioweapons as there is evidence of it being first used in the 14th century when it started the great Black Death in Europe that claimed 50 million lives. The plague can be deployed by a simple aerosol. Once a human is infected, they can quickly spread it to others, making the disease extremely dangerous and hard to control once it sets into motion. The Japanese army deployed fleas infected with plague over Manchuria during WWII. Russian scientists were also able to create a new strain of the plague that is resistant to antibiotics for weaponization in the 1980s.
The Marburg Virus
It is a category A virus that causes the deadly Marburg Hemorrhagic Fever. The virus has been traced to the African fruit bat. It can quickly be developed in the laboratory and experiments were conducted by Soviet scientists in the 1980s. It was found that the Marburg virus was responsible for Q fever and was the most potent with a high fatality rate of 90%.
Others
Other notable pathogens with the potential to be weaponized include the Bunyavirus which has three other strains, namely Nairovirus, Phlebovirus, and Hantavirus. Hantavirus causes the Korean hemorrhagic fever that killed more than 3,000 soldiers during the Korean War. Aflatoxins have also been used during the Gulf War by the Iraqi army although the impact was not widespread. Rice Blast Fungus is bioweapon that attacks food crops and is researched and developed by Russia and the United States during the cold war.
Dealing With Bioweapons
The use of bioweapons is strictly forbidden under customary international humanitarian law. However, it has not stopped many governments from conducting covert research into bioweapons. As of 2018, about 17 countries had a bioweapon program, including America, the UK, Canada, France, Germany, Israel, and Russia, among many others. Bioterrorism groups like the Aum Shinrikyo from Japan have for long spread fear with the threat of unleashing bioweapons in Tokyo. The danger that bioweapons pose has been the force behind many international accords and pacts signed in the last 100 years in a bid to reign in on the use of bioweapons. The 1925 Geneva Protocol banned the use of bioweapons in wars. The Biological Weapons Convention of 1972 went a step further and banned the production, acquisition, and stockpiling of bioweapons. The 180 states that were party to the convention were required to destroy any existing bioweapon stockpiles that they had. Governments around the world are now on alert as more terrorist groups turn their attention towards the use of bioweapons. Strict regulations have been passed to stamp out the menace.
Compiled & Shared by- Team, LITD (Livestock Institute of Training & Development)
Image-Courtesy-Google
Reference-On Request.